DEA Compliance: What You Need to Know About Drug Regulations and Safety
When you hear DEA compliance, the set of rules enforced by the U.S. Drug Enforcement Administration to control the distribution and use of addictive and dangerous drugs. Also known as controlled substance regulations, it's the backbone of how pharmacies, hospitals, and doctors handle everything from opioids to ADHD meds. It’s not just paperwork—it’s what stops pills from ending up on the street, keeps patients safe from dangerous interactions, and ensures that life-saving drugs like morphine or Adderall are only used when they’re truly needed.
DEA compliance ties directly into controlled substances, drugs classified by the DEA into five schedules based on abuse risk and medical value. Schedule II drugs, like oxycodone and fentanyl, have high abuse potential but are still used in hospitals and clinics under strict rules. DEA registration, the legal requirement for prescribers and pharmacies to register with the DEA to handle these drugs. Without it, a doctor can’t write a prescription for hydrocodone, and a pharmacy can’t dispense it. This system connects to real problems you’ll see in the posts below—like why generic drug shortages happen when manufacturers can’t get enough raw ingredients, or why some patients struggle to get pain meds even when they’re medically necessary.
It also links to pharmaceutical safety, the practice of ensuring medications are used correctly to avoid harm. When a patient takes clindamycin and gets C. diff, or mixes beta-blockers with the wrong supplements, DEA compliance helps track who prescribed what and when. It’s why pharmacies use electronic prescribing systems with built-in alerts, why doctors check state prescription databases before writing for benzodiazepines, and why you can’t just walk into a pharmacy and buy a month’s supply of Adderall without a valid, DEA-registered prescription.
DEA compliance isn’t about bureaucracy—it’s about balance. It lets people who need powerful drugs get them, while making it harder for misuse to slip through. The posts here show how this system plays out in real life: from the risks of first-generation antihistamines that can be abused, to the challenges of managing diabetes meds without triggering hypoglycemia, to how desensitization protocols for drug allergies require strict documentation to stay within legal bounds. You’ll see how medication errors are prevented with pill organizers, how pregnancy registries track fetal exposure, and why even something as simple as a cough syrup can fall under DEA rules if it contains codeine. This isn’t just about rules—it’s about protecting people, every day, in ways most never notice.
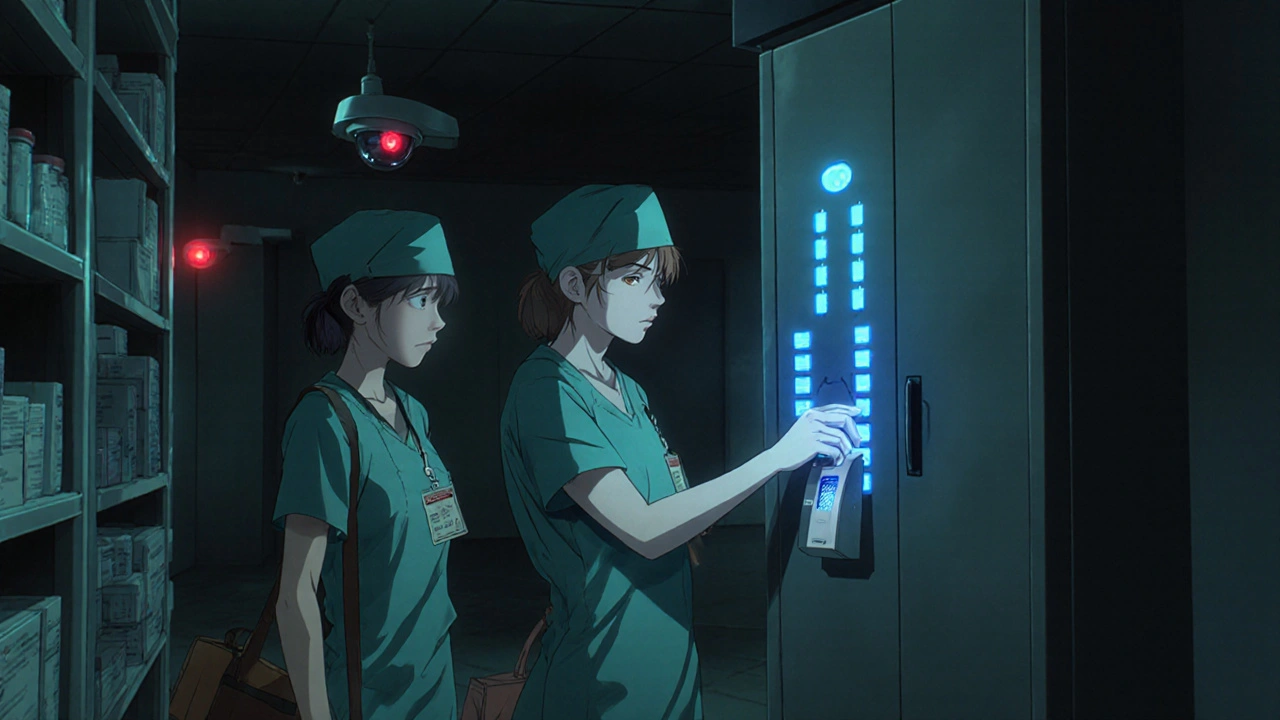
Learn how to securely store controlled substances to prevent theft and diversion in healthcare settings. Follow DEA-compliant practices, use dual control, implement audits, and avoid common pitfalls that put patients and staff at risk.

 Medications
Medications