When a single psychiatric medication doesn’t do the job, doctors often add another. This isn’t experimental-it’s standard practice. About 1 in 3 people with depression don’t respond to their first antidepressant. That’s why psychiatric medication combinations are used: an SSRI like sertraline paired with a low-dose antipsychotic like aripiprazole, or fluoxetine combined with olanzapine in a single pill called Symbyax. These combinations aren’t random. They’re backed by years of clinical trials and real-world use. But here’s the catch: when you switch from brand-name drugs to generics, things can go wrong-fast.
Why Combine Medications in the First Place?
Combination therapy isn’t about over-treating. It’s about precision. For someone with treatment-resistant depression, adding a low dose of aripiprazole to an SSRI can push remission rates from 11% to nearly 25%. That’s not a small gain-it’s life-changing. The same goes for bipolar disorder, where lithium or valproate is paired with an antipsychotic to control mood swings. Even anxiety disorders benefit: adding buspirone to an SSRI tackles lingering worry without the dependency risks of benzodiazepines. These combinations are carefully balanced. Each drug targets a different pathway. Too little, and symptoms return. Too much, and side effects overwhelm.
The FDA approved these combinations for a reason. Aripiprazole’s approval as an add-on to antidepressants in 2014 came after trials showed clear improvement in patients who had failed multiple treatments. Symbyax, approved in 2003, was one of the first fixed-dose combinations designed specifically to simplify treatment. But these successes rely on consistency. The exact amount of active ingredient, how slowly it’s released, even the shape of the pill’s coating-all matter.
Generic Substitution: The Hidden Risk
The FDA says generics are interchangeable. They must contain the same active ingredient and be 80-125% as bioavailable as the brand. Sounds fair. But for psychiatric drugs, that 45% window is a minefield. Think of it like this: if your blood pressure medication needs to stay within 10 points, and a generic can vary by 45 points, you’re gambling with your stability.
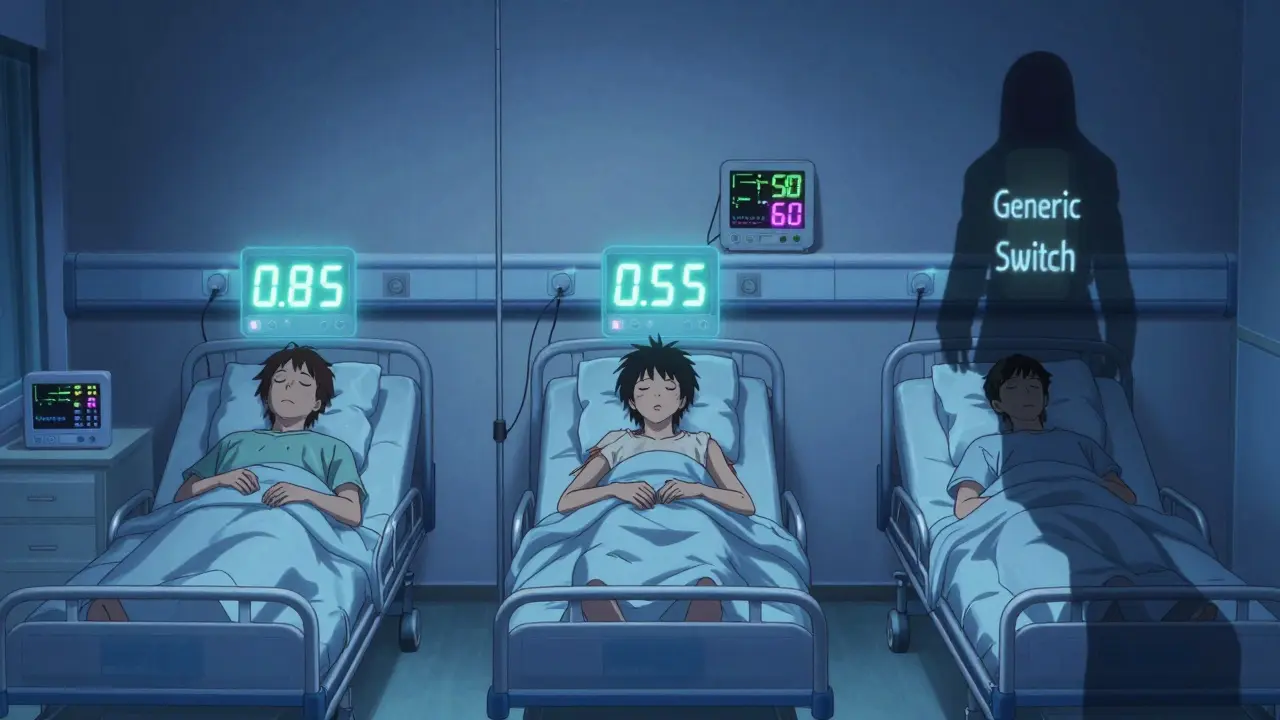
A 2019 study of nearly 28,500 patients found that switching from brand-name SSRIs to generics led to a 22.3% higher chance of treatment failure. That’s not a fluke. It’s a pattern. In one case series from the University of British Columbia, three bipolar patients went from stable to manic within two weeks of switching from brand-name lithium to a generic. Their blood levels dropped from 0.85 to 0.55 mmol/L-even though the dose didn’t change. Lithium’s therapeutic window is razor-thin: 0.6 to 1.2 mmol/L. A 0.3 drop isn’t just a number-it’s a relapse waiting to happen.
It’s not just lithium. Generic bupropion XL, the extended-release version of Wellbutrin, has been flagged by the FDA since 2012. Thirteen hundred adverse event reports detail mood crashes, panic attacks, and sudden anxiety after switching to certain generic versions. Why? The release mechanism is different. Brand-name Wellbutrin XL uses a precise osmotic system. Some generics use cheaper, inconsistent bead technology. The result? A patient gets too much drug too fast one day, too little the next. That’s not a difference. That’s instability.
Combination Therapy Makes It Worse
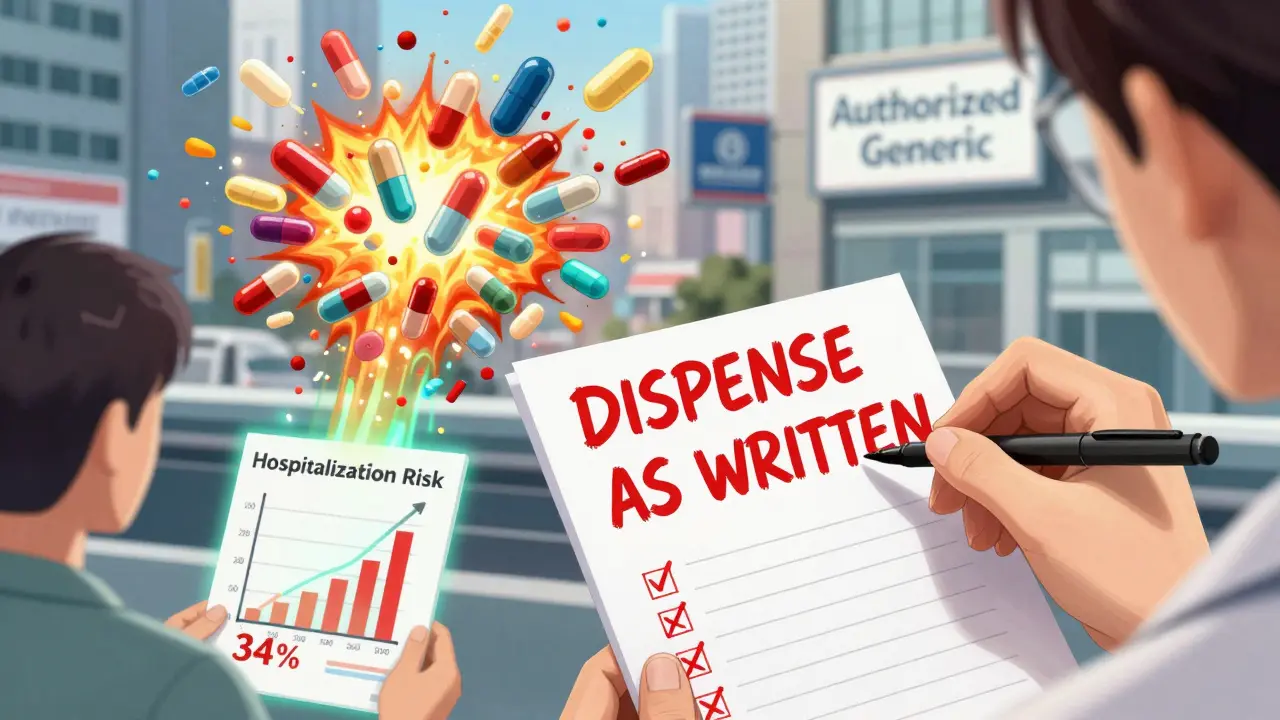
Here’s the real problem: combinations multiply the risk. If you’re on two drugs, and one of them has a 7% chance of causing a problem after a generic switch, you’re not just at 7%. You’re at higher risk because both drugs are now unpredictable. A 2020 study found that patients on combination therapy with lithium had a 34% higher chance of hospitalization after switching to a generic version. That’s not a coincidence. It’s a cascade.
Venlafaxine ER (Effexor XR) is another example. It works by balancing serotonin and norepinephrine in a 2:1 ratio. But different generic manufacturers use different bead systems. One might release serotonin faster. Another might delay norepinephrine. That changes the ratio. For someone on venlafaxine plus buspirone, even a small shift can undo months of progress. Patients report sudden irritability, sleeplessness, or worsening anxiety-symptoms that look like relapse, but are really just a bad generic.
Online communities are full of these stories. On Reddit’s r/depression, a top thread titled “Generic switch ruined my med cocktail” had over 1,200 upvotes. Users wrote about their Abilify stopping working after switching to a generic, or their Lamictal losing its effect. On PatientsLikeMe, 38.7% of people on combination therapy reported worsening symptoms after a generic switch-nearly three times higher than those on single drugs.
What Doctors Are Doing About It
Many clinicians are pushing back. The American Psychiatric Association’s 2022 guidelines say: “Switching between generic manufacturers may be as problematic as switching from brand to generic.” That’s bold. It means they’re not just warning-they’re advising against automatic substitution.
Hospitals like Massachusetts General and the University of Toronto have created tools to help. One tool scores risk based on three things: whether the drug has a narrow therapeutic index (3 points), if it’s part of a combination (2 points), and if the patient had a bad reaction to generics before (4 points). A score of 6 or higher? The system flags it. The prescriber gets a notification. No automatic switch.
Documentation matters too. Some psychiatrists now write the manufacturer and lot number on prescriptions. Why? Because in one 2021 case, a patient on lithium and carbamazepine had unexplained toxicity. The problem? A switch from Aurobindo to Mylan. The two generics had different absorption rates. The doctor knew because they’d recorded the manufacturer. Without that, it would’ve been impossible to trace.
The Cost vs. Safety Debate
Generics save money. In 2022, 89% of psychiatric prescriptions were generic. That’s $18.7 billion in savings. But what’s the hidden cost? A 2023 Congressional Budget Office report estimates that without changes, generic-related psychiatric hospitalizations will cost the system $2.4 billion annually by 2027. That’s more than the savings.
Some experts, like Dr. G. Caleb Alexander, argue that for most antidepressants, the risk is low. But even he admits: “Specific high-risk combinations, particularly those involving lithium or clozapine, warrant closer monitoring.” That’s the key. Not all drugs are equal. Not all substitutions are safe.
Insurance companies push for generics. Pharmacists are required to substitute unless the doctor says “do not substitute.” But what if the doctor doesn’t know? What if the patient doesn’t understand? The system is built for volume, not precision.
What You Can Do
If you’re on a combination therapy, here’s what matters:
- Ask your doctor: Is your medication on the list of high-risk generics? (Lithium, lamotrigine, bupropion XL, venlafaxine ER, carbamazepine)
- Check the pharmacy label: Look for the manufacturer name. If it changes unexpectedly, call your prescriber.
- Track your symptoms: Keep a simple log. Sleep? Mood? Energy? Irritability? A change in the first 10 days after a switch is a red flag.
- Request brand-name if needed: If you’re stable, ask for a “dispense as written” prescription. It’s legal. It’s your right.
Some pharmacies now offer authorized generics-brand-name drugs sold without the brand name at generic prices. Symbyax has one. So do a few other combinations. They’re not always cheaper, but they’re more consistent.
The Future Is Personalized
Things are changing. The FDA is drafting new rules: for combination drugs, they’re considering narrowing the bioequivalence range from 80-125% to 90-111%. That’s a big step. The Department of Veterans Affairs now requires patients on combination therapy to stay with the same generic manufacturer for at least a year. Preliminary data shows a nearly 19% drop in hospitalizations.
Long-term, pharmacogenetic testing could help. If your body metabolizes drugs a certain way, you might be told: “Stick with Aurobindo. Avoid Mylan.” That’s not science fiction-it’s coming by 2027. Until then, the safest approach is simple: if it works, don’t change it. And if you must change it, do it slowly, with eyes wide open.


 Medications
Medications