When fluid builds up in your belly because of liver disease, it’s not just uncomfortable-it’s a warning sign. This fluid buildup, called ascites, happens in about half of people with cirrhosis within 10 years. And once it shows up, your chances of living another two years drop by half. The good news? You can control it-with two powerful tools: cutting back on salt and taking diuretics. But here’s the twist: what doctors have told you for decades might not be the whole story anymore.
Why Ascites Happens
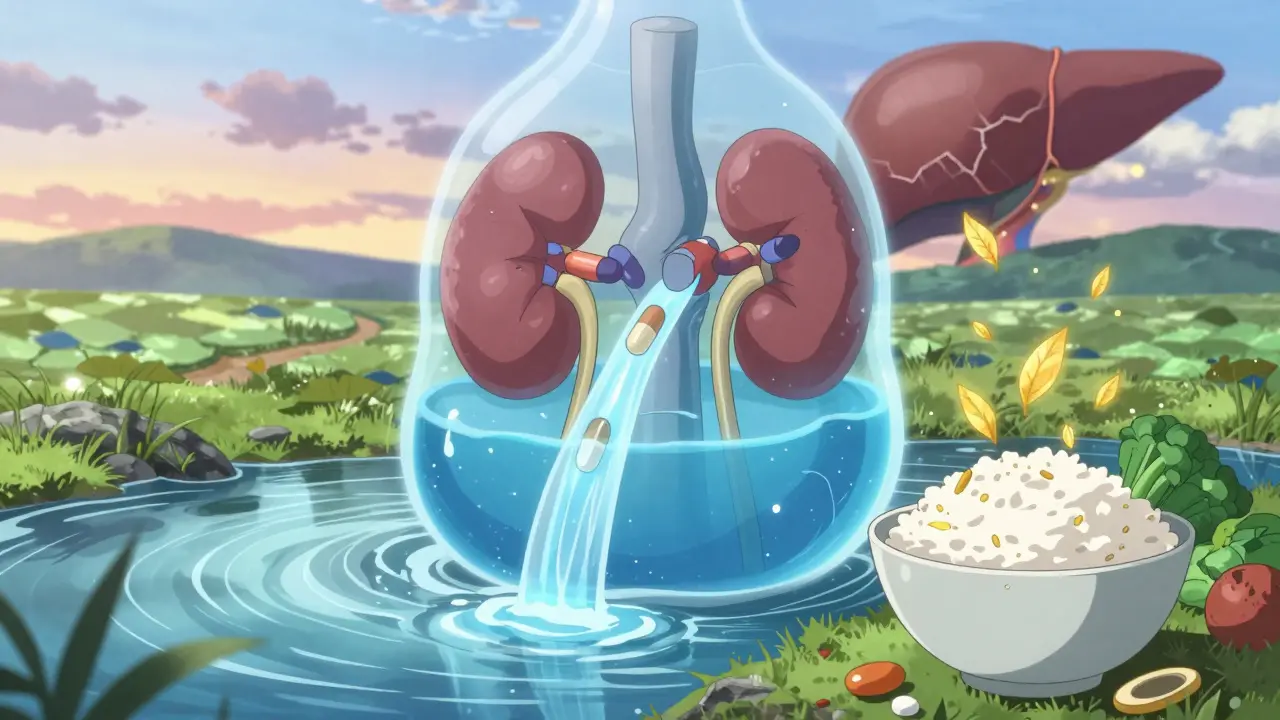
Ascites isn’t just water sitting in your belly. It’s the result of a broken system. When your liver is damaged by cirrhosis, blood flow through it gets blocked. That raises pressure in the portal vein-the main blood vessel feeding the liver. When that pressure hits 12 mmHg or higher, fluid starts leaking into your abdomen. At the same time, your kidneys start holding onto sodium like it’s gold. That sodium pulls water with it, and boom-fluid pools where it shouldn’t.
This isn’t random. It’s your body’s desperate attempt to fix low blood volume. But instead of helping, it makes things worse. The more fluid you retain, the more your body tries to hold on, creating a cycle that’s hard to break without intervention.
Sodium Restriction: The Old Rule and the New Debate
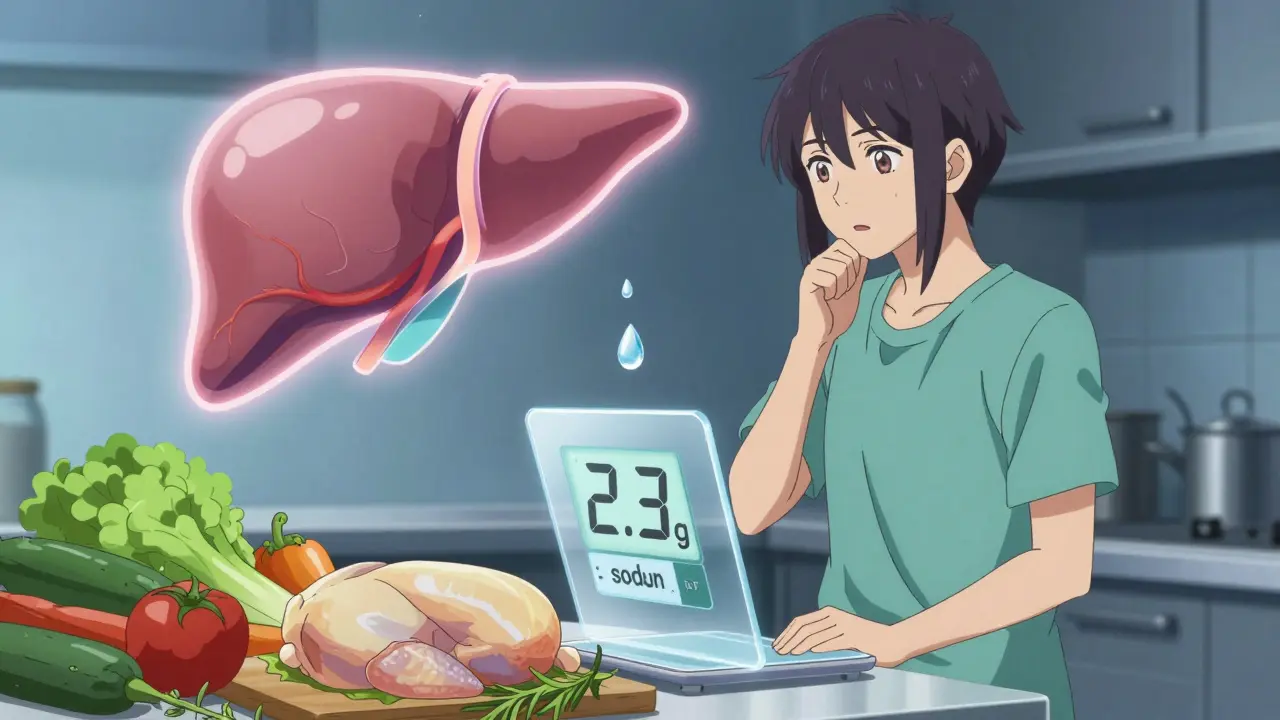
For years, doctors told patients with ascites to eat less than 2 grams of sodium a day. That’s about 5 grams of salt-roughly one teaspoon. It sounds simple. But try doing it. Most of the sodium you eat doesn’t come from the salt shaker. It’s in bread, canned soup, deli meats, sauces, and even breakfast cereal. A 2021 study found fewer than 4 in 10 patients could stick to that limit.
And now, new research is shaking things up. Two major trials from 2017 to 2022 found that people who ate 5 to 6.5 grams of salt a day (about 2 to 2.5 grams of sodium) actually had better outcomes than those on strict low-sodium diets. Their ascites resolved in 45% of cases, compared to just 16% in the strict restriction group. They also needed fewer procedures to drain fluid from their bellies.
Why? Because going too low can backfire. When you cut sodium too hard, your kidneys don’t get enough blood flow. That can trigger something called hepatorenal syndrome-a dangerous drop in kidney function that’s already a risk in cirrhosis. One study showed severe sodium restriction pushed that risk from 18% to 35%.
So what’s the real answer? Experts are split. Dr. Guadalupe Garcia-Tsao, who helped write the American guidelines, still says 2 grams is the target. But Dr. Pere Gines, who led the 2022 study, says strict restriction may actually hurt more than help. Dr. Frederick Wong from Toronto suggests a middle ground: aim for 5 to 6.5 grams of salt daily-not zero, not unlimited. That’s about 1.5 to 2.5 grams of sodium. It’s enough to avoid kidney strain, but still helps diuretics work better.
Diuretics: The Engine That Drains the Fluid
Sodium restriction alone doesn’t do enough. That’s where diuretics come in. These are pills that tell your kidneys to flush out extra salt and water. The two main ones used are spironolactone and furosemide.
Spironolactone is the first-line drug. You start with 100 mg a day, and if it’s not working after three days, your doctor may bump it up-every 72 hours-until you hit 400 mg. It works slowly but steadily. Furosemide is added if you’re still retaining fluid. You start with 40 mg and can go up to 160 mg. The combo is usually reserved for people who’ve had ascites before or who aren’t responding to spironolactone alone.
Here’s the key: you don’t want to lose weight too fast. If you have swelling in your legs, you can safely lose up to 1 kg (2.2 lbs) per day. If you don’t have swelling, stick to 0.5 kg (1 lb) per day. Losing weight too fast can crash your blood pressure or hurt your kidneys.
And you need to watch your blood sodium levels. About one in three people with ascites already have low sodium. If it drops below 130, your doctor will adjust your diuretics and maybe limit fluids. If it’s too low and you’re dehydrated, you might need IV saline and lower diuretic doses.
What Not to Take
Some common medications can make ascites worse. Avoid NSAIDs like ibuprofen or naproxen. They reduce blood flow to the kidneys and can trigger kidney failure in people with cirrhosis. ACE inhibitors and ARBs-used for high blood pressure-are also risky. Studies show they raise the chance of end-stage kidney disease by more than double in cirrhosis patients.
Even over-the-counter painkillers can be dangerous. Always check with your doctor before taking anything new. Your liver is already working overtime. Don’t make it harder.
When Diuretics Don’t Work
Five to ten percent of people with ascites don’t respond to maximum doses of diuretics. This is called refractory ascites. For them, draining the fluid with a needle-called large-volume paracentesis-is the next step. Doctors remove up to 5 liters at a time and give back albumin (a blood protein) to keep blood pressure stable. It’s effective, but it needs to be done in a hospital, and there’s a 5-10% risk of infection or bleeding.
There are other drugs, like vaptans, that block water retention. But they cost $5,000 to $7,000 a course and can only be used for 30 days. They’re not practical for most people.
The Bigger Picture: Personalized Care
The old one-size-fits-all approach to sodium is fading. Hepatologists today are moving toward individualized plans. At the 2022 AASLD meeting, 65% of doctors said they adjust sodium limits based on the patient’s kidney function, appetite, and overall health-not just a rigid number.
Why? Because many people with cirrhosis are malnourished. Between 35% and 90% lack enough protein and calories. If you’re so focused on cutting salt that you stop eating, you’re trading one problem for another. Your body needs fuel to heal. Sometimes, a slightly higher salt intake that lets you eat more is better than a strict diet that leaves you weak.
Future studies like the PROMETHEUS trial (NCT04567890), expected to finish in late 2025, may finally settle the debate. Until then, the best approach is this: work with your doctor to find the lowest sodium level you can stick to without losing your appetite or energy-and pair it with the right diuretic dose.
What You Can Do Today
- Check food labels. Look for sodium content-not salt. 1 gram of sodium = 2.5 grams of salt.
- Avoid processed foods. Choose fresh meats, vegetables, and plain grains.
- Use herbs and lemon instead of salt for flavor.
- Take diuretics exactly as prescribed. Don’t skip doses or double up.
- Track your weight daily. A sudden gain of 2 kg (4.4 lbs) in a week means fluid is building up.
- Get your blood sodium checked at least twice a week when starting treatment.
- Never take NSAIDs or blood pressure meds without your doctor’s approval.
Ascites is serious, but it’s manageable. It’s not about perfection. It’s about balance. Enough salt to keep your kidneys working, enough diuretics to drain the fluid, and enough nutrition to keep your body strong. That’s the new standard.
Can I ever eat salt again if I have ascites?
Yes-but not freely. Most experts now recommend moderate salt restriction: 5 to 6.5 grams of salt per day (2 to 2.5 grams of sodium). That’s about 1 to 1.5 teaspoons of table salt. Avoid processed foods, and focus on whole, unseasoned meals. The goal isn’t zero sodium-it’s enough to help diuretics work without harming your kidneys.
Why do I need to weigh myself every day?
Daily weight is the best early warning sign for fluid buildup. A gain of more than 1 kg (2.2 lbs) in a day or 2 kg (4.4 lbs) in a week means your body is holding onto fluid again. That’s your cue to check your salt intake, take your diuretics, or call your doctor. It’s simple, cheap, and saves lives.
Are diuretics safe for long-term use?
Yes, when monitored properly. Spironolactone and furosemide are safe for years if your kidney function and electrolytes are checked regularly. The biggest risks are low potassium, low sodium, or kidney stress-none of which happen if you’re getting blood tests every few weeks when starting out. Your doctor will adjust doses as needed.
What if I can’t afford the prescribed diuretics?
Spironolactone is available as a low-cost generic. Furosemide is also inexpensive. If cost is an issue, talk to your doctor or pharmacist. Many hospitals have medication assistance programs. Never skip doses because of cost-there are alternatives, and your doctor can help you find them.
Can ascites go away completely?
In early stages, yes-if you follow treatment closely. Up to 90% of people with uncomplicated ascites see significant improvement with sodium control and diuretics. But if cirrhosis is advanced, ascites often returns. That doesn’t mean treatment failed. It means the liver damage is ongoing. The goal then shifts from curing ascites to managing it safely and avoiding complications like infection or kidney failure.
Does drinking less water help with ascites?
Only in specific cases. If your blood sodium is very low (below 125 mEq/L) and you’re retaining water, your doctor might limit fluids to 1 liter a day. But for most people, normal fluid intake is fine-and even encouraged. Dehydration makes kidney problems worse. Don’t restrict water unless your doctor tells you to.
What’s the biggest mistake people make with ascites?
Trying to do it alone. Ascites isn’t just about diet or pills. It’s about monitoring, communication, and timing. Waiting until your belly is swollen to call your doctor is too late. Daily weight checks, regular blood tests, and open communication with your care team are what keep you out of the hospital.

 Medications
Medications
Joy Nickles
January 1, 2026 AT 10:39Emma Hooper
January 3, 2026 AT 04:01Marilyn Ferrera
January 4, 2026 AT 01:09John Chapman
January 5, 2026 AT 08:05Urvi Patel
January 6, 2026 AT 18:12anggit marga
January 7, 2026 AT 22:39Martin Viau
January 9, 2026 AT 07:00Robb Rice
January 10, 2026 AT 20:23Harriet Hollingsworth
January 11, 2026 AT 10:43Deepika D
January 13, 2026 AT 06:44Bennett Ryynanen
January 14, 2026 AT 03:09