Why Generic Drugs Keep Running Out
It’s 3 a.m. in the ER. A patient needs an antibiotic to fight a life-threatening infection. The shelf is empty. The pharmacy calls three distributors. Nothing. A backup drug is found-but it’s not as effective, and the patient’s condition worsens. This isn’t rare. It happens every day across the U.S. And it’s not because of a lack of need. It’s because the system keeping generic drugs in stock has broken.
Generic drugs make up 90% of all prescriptions filled in the U.S. But they’re also behind 95% of all drug shortages. These aren’t rare glitches. They’re structural failures. And they’re getting worse.
Manufacturing Problems Are the #1 Cause
Over 60% of all drug shortages since 2020 have been caused by manufacturing issues. Not bad luck. Not bad weather. Not a sudden spike in demand. It’s contamination, equipment breakdowns, and quality control failures at factories that produce these drugs.
Imagine a single factory in India making the only sterile injectable version of a chemotherapy drug used in hospitals nationwide. One leak in a sterilization system. One batch of contaminated product. The FDA shuts the line down. No backups. No spare capacity. The drug vanishes from shelves for months. That’s not hypothetical. That’s happened with drugs like doxorubicin, cisplatin, and propofol.
These aren’t small operations. These are high-tech, sterile facilities that cost hundreds of millions to build and maintain. But because generic drugs sell for pennies, manufacturers cut corners. They delay upgrades. They skip routine maintenance. They stretch staff thin. One small error-like a filter that wasn’t replaced-can shut down production for weeks. And when you’re running at 98% capacity with zero buffer, there’s no room to recover.
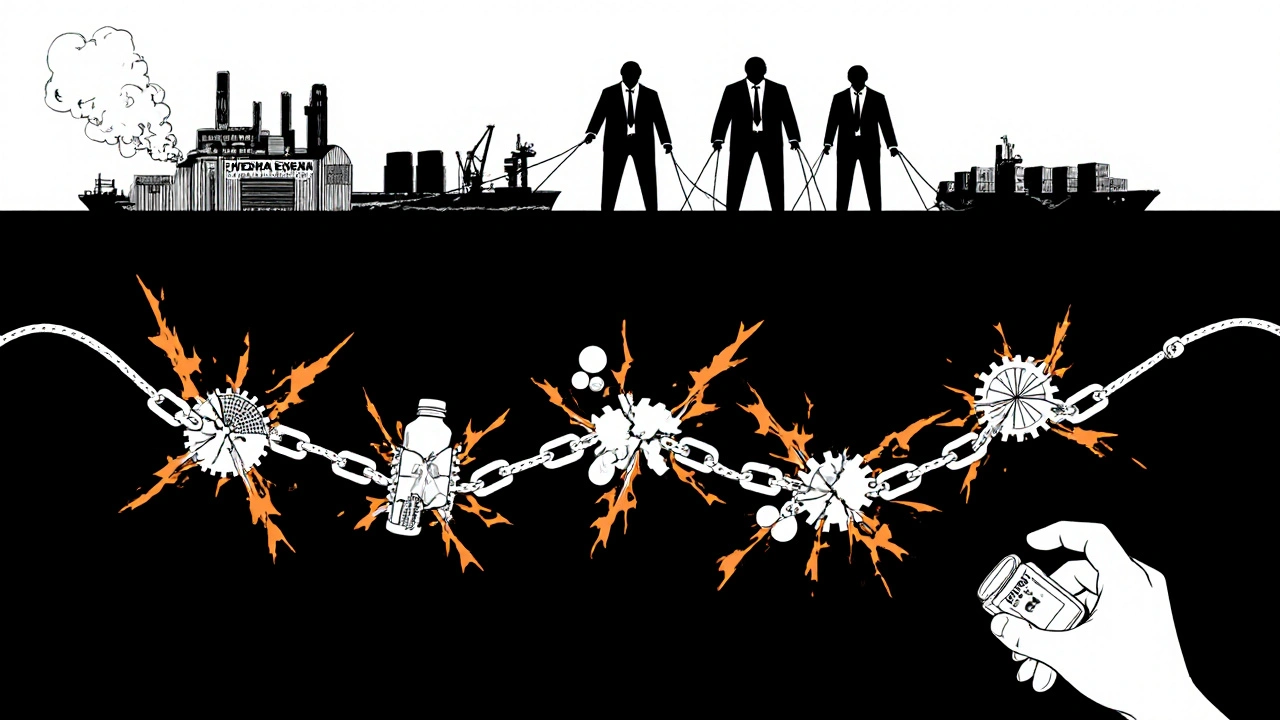
Global Supply Chains Are Fragile
Eighty percent of the active ingredients (APIs) in U.S. generic drugs come from just two countries: China and India. That’s not diversity. That’s dependency.
When a factory in Shanghai shuts down for environmental violations, or a port in Mumbai gets backed up due to labor strikes, the ripple effect hits U.S. hospitals. In 2020, during the pandemic, lockdowns in India delayed shipments of heparin, insulin, and antibiotics. Hospitals scrambled. Patients waited. Some died.
And it’s not just about shipping. It’s about control. A single company might own the API plant in India, the formulation lab in the Philippines, and the final packaging facility in Mexico. If any one link breaks, the whole chain fails. There’s no redundancy. No backup supplier. No Plan B.
Compare that to branded drugs, where companies keep multiple manufacturing sites and stockpile raw materials. Generic manufacturers? They run lean. Too lean. They don’t keep extra inventory because there’s no profit in it.
No One Makes Extra-Because No One Gets Paid For It
Generic drugs are cheap. Really cheap. A 30-day supply of amoxicillin might cost $4. A vial of epinephrine? $1.50. That’s great for consumers-but terrible for manufacturers.
Branded drugs can make 30-40% profit margins. Generics? Often under 15%. Sometimes less than 5%. That’s not enough to invest in new equipment, hire extra staff, or keep spare inventory. So manufacturers don’t. They run at full tilt, every day, with no safety net.
And when one company stops making a drug-because the price dropped too low or the FDA flagged quality issues-no one else steps in. Why? Because entering the market means investing millions to pass FDA inspections, then competing with 10 other companies already selling the same drug for pennies. The return on investment? Years of losses before you break even.
Since 2010, over 3,000 generic drugs have been discontinued. Most weren’t recalled. They just disappeared because no one could make money on them anymore.
Pharmacy Benefit Managers Control the Market-and Make It Worse
Three companies-CVS Caremark, Express Scripts, and OptumRx-control about 85% of prescription drug spending in the U.S. They’re called pharmacy benefit managers, or PBMs. They don’t make drugs. They don’t dispense them. But they decide which drugs get covered, and at what price.
Here’s how it works: PBMs demand the lowest possible price from manufacturers. They threaten to exclude a drug from their formulary if the price isn’t low enough. Manufacturers lower prices. Then they cut costs-on quality, on staffing, on maintenance. Then they get shut down by the FDA. Then the drug goes into shortage.
And when a shortage happens? PBMs often don’t tell hospitals or doctors. They just switch the default drug on the system. But the alternative might be less effective, harder to use, or in shortage too. Hospitals are left guessing why a drug disappeared-and how to replace it.
The Federal Trade Commission called this lack of transparency “unacceptable.” But nothing’s changed. PBMs still operate without public oversight. And the cycle continues.
One Supplier, One Product, One Disaster
One in five drug shortages involve a product made by a single manufacturer. That’s called sole-sourcing. And it’s a ticking time bomb.
Take the drug sodium bicarbonate, used in emergency rooms for heart attacks and kidney failure. For years, only one company made it in the U.S. When their plant had a power outage, the drug vanished. No one else could make it fast enough. Patients were put on dialysis longer. Others got delayed care.
Why does this happen? Because PBMs pushed prices so low that no other company could profitably enter the market. The original maker stayed in business-not because they were the best, but because they were the only one left.
It’s like having one bridge to your city. If it breaks, you’re stuck. That’s not infrastructure. That’s a gamble with people’s lives.
Why Canada Doesn’t Have This Problem
Canada has a similar generic drug market. Same active ingredients. Same manufacturers. Same global supply chains. But they have far fewer shortages.
Why? Because they don’t leave it to the market. Canada has a national drug stockpile. It’s not just for bioterrorism or pandemics-it’s for everyday drug shortages. When a drug runs low, the government steps in, buys extra, and redistributes it.
They also force manufacturers, pharmacies, and hospitals to share real-time data. If a drug is running low in Toronto, Ottawa knows within hours. They can redirect supply. In the U.S.? No such system exists. Hospitals don’t even know why a drug is gone-40% of shortage reports have no stated cause.
Canada’s system isn’t perfect. But it’s designed to protect patients. Ours is designed to cut costs.
What’s Being Done? Not Enough
There’s a bill in Congress called the RAPID Reserve Act. It proposes creating a federal stockpile of critical generic drugs. It would give tax breaks to manufacturers who produce them in the U.S. It would require companies to report potential shortages earlier.
It’s a start. But it’s not enough.
Real change means paying manufacturers more for low-margin drugs. It means forcing PBMs to be transparent. It means requiring backup suppliers for essential medicines. It means building manufacturing capacity here, not just importing from halfway across the world.
Until then, the same cycle will keep repeating: a drug disappears. A patient suffers. A doctor scrambles. And nothing changes.
What You Can Do
If you take generic drugs regularly, keep track of what you use. If your pharmacy says a drug is unavailable, ask why. Demand to know if there’s an alternative-and if it’s safe. Talk to your doctor. Ask if there’s a different brand or formulation that’s still in stock.
And if you’re a healthcare worker, speak up. Report shortages to your hospital’s pharmacy committee. Push for better communication. Demand transparency.
This isn’t just a supply chain problem. It’s a human problem. And it only gets worse when no one talks about it.


 Medications
Medications
katia dagenais
November 24, 2025 AT 15:03Josh Gonzales
November 26, 2025 AT 06:54Jack Riley
November 27, 2025 AT 12:30Jacqueline Aslet
November 28, 2025 AT 06:59Caroline Marchetta
November 29, 2025 AT 06:07Valérie Siébert
December 1, 2025 AT 05:41Ellen Sales
December 2, 2025 AT 19:35Josh Zubkoff
December 3, 2025 AT 20:43fiona collins
December 5, 2025 AT 09:27Andrew McAfee
December 6, 2025 AT 06:56Erika Hunt
December 7, 2025 AT 10:09prasad gaude
December 7, 2025 AT 15:37