Every time you pick up your prescription, you might get a different pill. Same active ingredient. Different color. Different shape. Different brand name on the bottle. This isn’t a mistake. It’s generic switching-and it’s happening more often than you think.
In Australia, the U.S., and most developed countries, over 80% of prescriptions are filled with generic drugs. That’s because they cost up to 85% less than brand-name versions. But here’s the catch: not all generics are made the same. And when your pharmacy switches from one generic manufacturer to another-sometimes month to month-it can actually affect how the medicine works in your body.
Why Do Generic Switches Happen?
It’s not about your doctor or your pharmacy trying to confuse you. It’s about money and supply chains.
Insurance companies and government programs push for the cheapest option. Pharmacies get bulk discounts from manufacturers who bid the lowest. If Teva’s version of your blood pressure pill is $5 this month and Mylan’s is $3 next month, your pharmacy will switch-without telling you.
Drug shortages also force switches. If one manufacturer can’t keep up, the pharmacy grabs whatever’s available. And with over 4.3 generic versions on average for each off-patent drug, there’s always a backup.
But here’s what most people don’t realize: just because two generics have the same active ingredient doesn’t mean they behave the same way in your body.
The Bioequivalence Myth
The FDA says generics must be “bioequivalent” to the brand-name drug. That means they deliver between 80% and 125% of the active ingredient compared to the original. Sounds strict, right?
Here’s the problem: if Generic A delivers 80% and Generic B delivers 125%, that’s a 45% difference between the two. For most drugs, that’s fine. Your body can handle it. But for some, it’s dangerous.
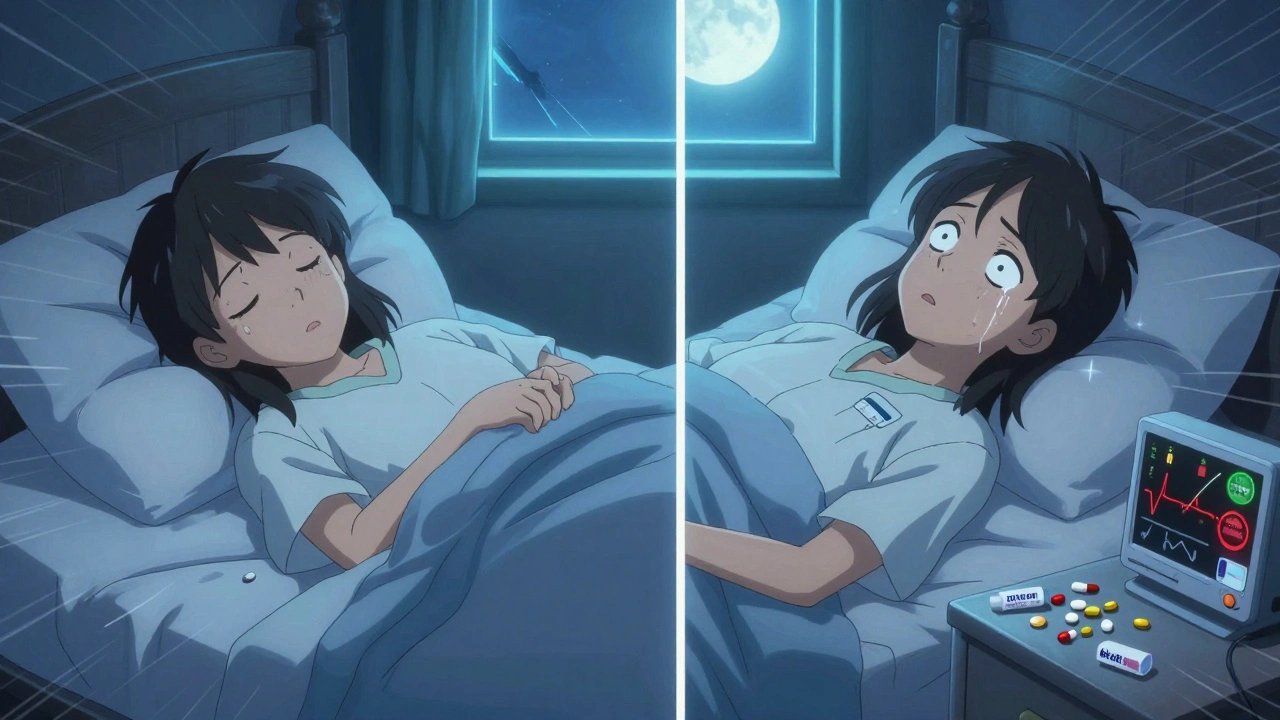
These are called narrow therapeutic index (NTI) drugs. They have a tiny window between working and causing harm. Even a small change in blood levels can lead to serious side effects-or make the drug stop working entirely.
Common NTI drugs include:
- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Tacrolimus (transplant rejection drug)
- Phenytoin and carbamazepine (seizure medications)
For these, switching between generics isn’t just inconvenient-it’s risky.
Real Stories: When Switching Goes Wrong
One patient in Melbourne, on levothyroxine for 12 years, told her doctor: “Every time the pill changes, I feel like I’m getting sick again. Fatigue, weight gain, brain fog. It takes weeks to feel normal after each switch.”
Her TSH levels jumped every time her pharmacy switched manufacturers. Her endocrinologist had to adjust her dose three times in six months. She finally asked her pharmacist to lock her on one brand-and it stabilized.
Another patient, on carbamazepine for epilepsy, had two seizures after his pharmacy switched from one generic to another. His neurologist checked his blood levels: they’d dropped 30%. He’d been stable for years. Then the pill looked different. Then he had seizures.
On the flip side, many people switch generics with no issues. People on statins, antibiotics, or even lisinopril often report zero changes. But those are not NTI drugs. The body has room to absorb the variation.
Which Drugs Are Safe to Switch? Which Aren’t?
Not all medications are created equal. Here’s a quick guide based on real-world data:
| Drug Class | Switching Risk | Why |
|---|---|---|
| Levothyroxine | High | Small changes in blood levels cause major thyroid symptoms. Even 10% variation can trigger fatigue or heart palpitations. |
| Warfarin | High | INR levels fluctuate after switches. One study showed 28% of patients needed dose changes within 30 days of a generic change. |
| Antiepileptics | High | Up to 44% of patients report breakthrough seizures after switching. Blood levels drop or spike unpredictably. |
| Tacrolimus | Very High | Transplant patients can reject organs if levels drop. Dose adjustments are often needed after every switch. |
| Statins | Low | Cholesterol levels stay stable across generics. No significant clinical difference found in studies. |
| Antihypertensives (e.g., lisinopril) | Low | Most patients maintain stable blood pressure regardless of manufacturer. |
| Antibiotics | Very Low | Short-term use. Body clears them quickly. Variation doesn’t impact outcomes. |
Bottom line: if your drug is on the “High” or “Very High” list, you need to be careful. Don’t assume it’s safe just because it’s generic.
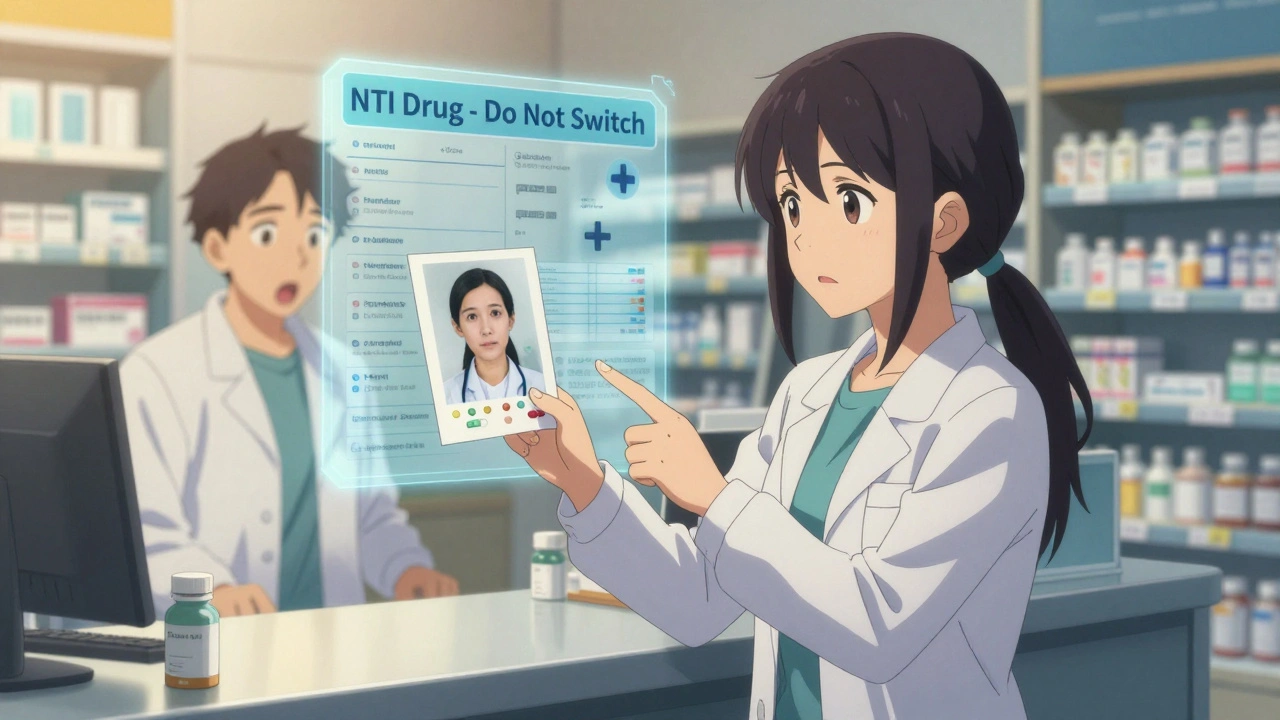
What You Can Do to Protect Yourself
You don’t have to accept random switches. Here’s how to take control:
- Ask your pharmacist every time you pick up your prescription: “Is this the same manufacturer as last time?” Write down the name on the bottle. If it changes, ask why.
- Request a “lock-in” for NTI drugs. Many pharmacies can hold your prescription to one specific generic manufacturer. You may need a note from your doctor.
- Check your pill. Take a photo of your pill the first time you get it. If the color, shape, or imprint changes, don’t just take it. Call your pharmacist.
- Get blood tests after any switch. If you’re on warfarin, get an INR check 7-10 days after a new generic. For levothyroxine, check TSH 4-6 weeks after a switch.
- Talk to your doctor. Tell them you’ve had issues with switching. Ask if your drug is high-risk. Some doctors don’t know about the risks unless you bring it up.
One patient in Sydney told his GP: “I don’t care if it costs $2 more. I need the same pill every month.” His doctor wrote “Dispense as written” on the prescription. That legally stops the pharmacist from switching without permission.
Why Doctors Don’t Always Know
A 2023 survey found that 62% of doctors didn’t know when their patients switched generics. Why? Because pharmacies don’t notify them. Insurance systems auto-substitute. Patients don’t realize it’s a problem until they feel off.
That’s why you have to be your own advocate. If your medication isn’t working the same way, or you’re feeling worse, don’t assume it’s “just your condition.” Ask: “Could this be the pill?”
What’s Changing in the Future
Regulators are starting to wake up. In June 2024, Medsafe (Australia’s drug regulator) issued new guidance: “Avoid switching between different brands of levothyroxine where possible.”
The FDA launched a pilot program in 2023 requiring generic manufacturers to report any formulation changes. Some U.S. hospitals now use “lock-in” systems for transplant and epilepsy patients.
There’s also a push for standardized pill designs-so all generics for the same drug look the same, no matter who makes them. That would cut down on confusion.
But until then, the system still favors cost over consistency. And if you’re on a high-risk drug, that gap can be dangerous.
Final Thoughts: It’s Not About Generic vs. Brand-It’s About Consistency
Generics are safe and effective for most people. They’ve saved billions in healthcare costs. That’s not the issue.
The issue is switching-frequently, without warning, without monitoring-between different versions of the same drug. That’s where the risk creeps in.
If you’re on a statin or an antibiotic, you’re probably fine. But if you’re on warfarin, levothyroxine, or an antiseizure drug, don’t treat generics like interchangeable commodities. Your body isn’t a vending machine. It needs stability.
Ask questions. Track your pills. Get tested. Speak up. You have the right to know what’s in your medicine-and to demand consistency when it matters most.


 Medications
Medications
Rebecca M.
December 2, 2025 AT 20:05Oh wow, so my thyroid meds are basically a Russian roulette pill now? Thanks for the heads-up, I guess. I’ve been wondering why I feel like a zombie every other Tuesday. 🙃
Lynn Steiner
December 4, 2025 AT 07:44I’m so tired of this. I’ve been on levothyroxine for 15 years and every time the pill changes color, I feel like I’m dying. My doctor doesn’t care. Insurance doesn’t care. Everyone just wants the cheapest option. I’m not a number. I’m not a cost center. I’m a person. 😔
Alicia Marks
December 5, 2025 AT 06:28You got this. Ask for the lock-in. Take a photo of your pill. Track your symptoms. Small steps = big wins. You’re not alone. 💪
Paul Keller
December 6, 2025 AT 09:05While the piece presents a compelling case for pharmaceutical consistency, particularly with regard to narrow therapeutic index drugs, it is imperative to contextualize this within the broader framework of healthcare economics. The systemic pressure to reduce expenditures through generic substitution is not inherently nefarious; rather, it is a logical outcome of market forces amplified by regulatory frameworks designed to maximize access. That said, the absence of mandatory notification protocols and the lack of pharmacovigilance integration between pharmacy and prescriber systems represent critical gaps in patient safety infrastructure. A standardized, interoperable digital tracking system for generic dispensing-linked to EHRs-would mitigate risk without sacrificing cost-efficiency. The solution lies not in rejecting generics, but in refining their deployment.
Steve Enck
December 7, 2025 AT 00:17Let us not conflate bioequivalence with therapeutic equivalence. The FDA’s 80–125% window is a statistical artifact, not a physiological guarantee. It is a regulatory compromise born of industrial pragmatism, not medical wisdom. When we treat human physiology as a variable in a supply chain optimization algorithm, we are no longer practicing medicine-we are operating a logistics network with a side of placebo. The patient is the dependent variable. And we are losing them, one pill switch at a time.
Jay Everett
December 7, 2025 AT 00:35Bro, this is wild. I’m on warfarin and I started taking pics of my pills after a switch made me dizzy for a week. Now I keep a little notebook: ‘Pill A – blue oval, ‘Teva’ – stable INR. Pill B – white circle, ‘Mylan’ – INR spiked to 5.2.’ My pharmacist thinks I’m nuts. I’m like, ‘Nah, you’re the one who doesn’t know what’s in my blood.’ 🤓💉
मनोज कुमार
December 7, 2025 AT 01:29Roger Leiton
December 7, 2025 AT 11:34This is so important. I didn’t even realize my blood pressure meds switched until I started getting headaches. Now I always check the bottle. I even showed my mom how to take a photo of her pill so she doesn’t get confused. 📸❤️
Laura Baur
December 8, 2025 AT 01:39It is not merely a matter of pharmaceutical inconsistency-it is a profound epistemological failure of the modern healthcare system. We have outsourced therapeutic identity to corporate bidding wars and automated substitution protocols, thereby abdicating our responsibility to maintain the integrity of the patient’s physiological narrative. The pill is no longer a therapeutic agent; it is a commodified token in a neoliberal transaction. The patient’s lived experience is rendered irrelevant unless it is quantifiable in lab values. This is not healthcare. This is pharmaceutical capitalism with a side of denial.
Arun kumar
December 8, 2025 AT 07:23Zed theMartian
December 9, 2025 AT 01:25Oh, so the system is broken? Shocking. Next you’ll tell me the moon landing was faked or that pineapple doesn’t belong on pizza. I’m just glad I can afford my $400 brand-name pills while you peasants are playing Russian roulette with your thyroid. 🤡
ATUL BHARDWAJ
December 10, 2025 AT 13:52Steve World Shopping
December 10, 2025 AT 21:04