Most people don’t feel metabolic syndrome coming. No sharp pain. No sudden dizziness. Just a slowly tightening belt, a quiet rise in blood pressure readings, and a blood test that shows triglycerides climbing while good cholesterol drops. By the time symptoms show up, the damage is already building-inside your arteries, your liver, your pancreas. Metabolic syndrome isn’t a disease you catch. It’s a slow burn, fueled by everyday choices, and it affects one in three adults in the U.S. right now. And if you’re over 50, that number jumps to nearly half.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome isn’t one thing. It’s five warning signs that show up together: too much belly fat, high blood pressure, high triglycerides, low HDL cholesterol, and elevated blood sugar. You don’t need all five. Just three. That’s all it takes for your risk of heart attack, stroke, or type 2 diabetes to jump by 1.5 to 2 times.
The term was first called "Syndrome X" in 1988 by Dr. Gerald Reaven, who noticed that people with insulin resistance kept showing up with this same pattern: fat around the middle, high blood pressure, and messed-up fats in their blood. Today, we know it’s not just a coincidence. It’s a system failure.
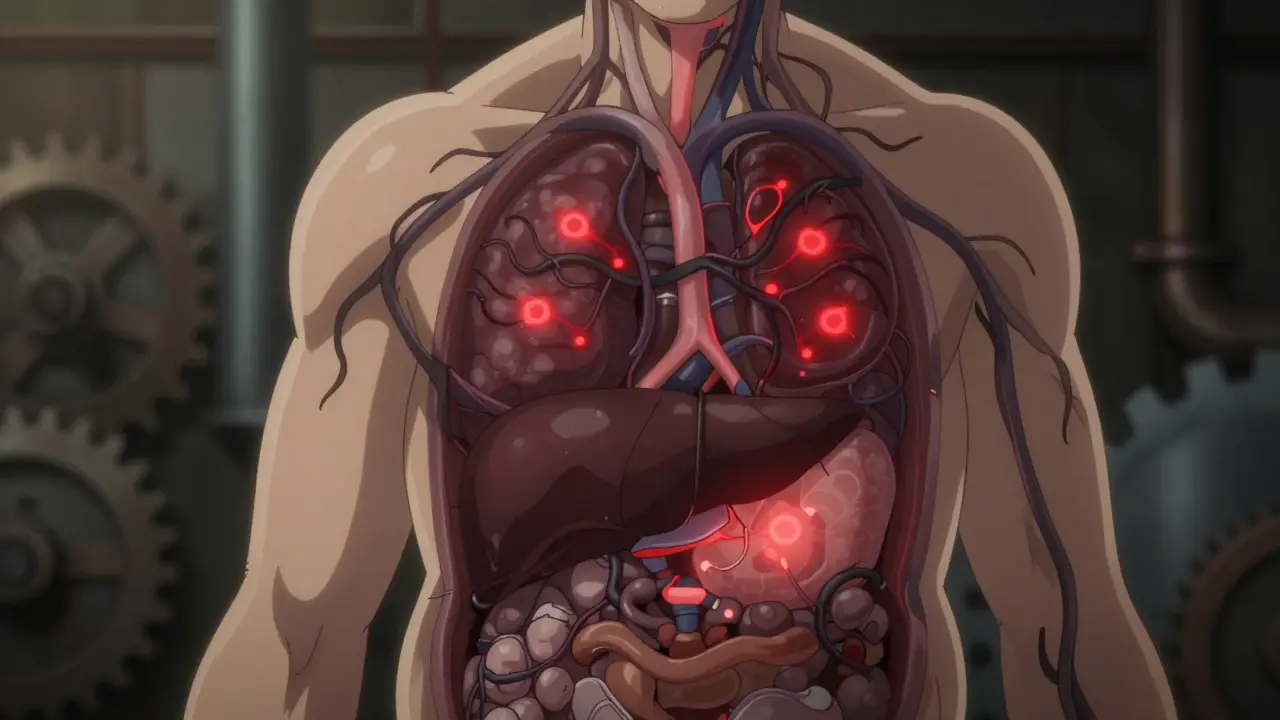
Think of your body like a factory. Insulin is the key that unlocks cells so glucose can enter and be used for energy. When you carry too much fat-especially deep inside your belly-those fat cells start leaking chemicals. They flood your bloodstream with fatty acids and inflammatory signals. Your cells become blind to insulin. The pancreas pumps out more and more to compensate. Blood sugar rises. Triglycerides pile up. HDL drops. Blood pressure climbs. The factory is clogged, and everything starts to break down.
Abdominal Obesity: The Visible Red Flag
Not all fat is the same. Fat under your skin (subcutaneous) is mostly harmless. Fat wrapped around your organs (visceral) is dangerous. That’s the kind that defines metabolic syndrome. It’s measured by waist circumference.
In the U.S. and Europe, the cutoffs are clear:
- Men: more than 102 cm (40 inches)
- Women: more than 88 cm (35 inches)
But these numbers change depending on your ethnicity. For people of South Asian, Chinese, or Japanese descent, the risk starts lower: 90 cm for men, 80 cm for women. Why? Because even at a "normal" weight, these populations tend to store more fat internally. A person who looks thin but has a waist over 90 cm can still be at high risk.
Here’s the thing: you can’t see insulin resistance. But you can see a growing waistline. If your belt keeps needing to be tightened-and you’re not intentionally gaining muscle-you’re likely carrying visceral fat. And that’s your body’s loudest alarm.
High Blood Pressure: The Silent Pressure
Normal blood pressure? Less than 120/80 mmHg. If you’re at 130/85 or higher, you’re in the danger zone for metabolic syndrome. And here’s the catch: most people with high blood pressure feel nothing. No headaches. No ringing in the ears. Just a number on a screen that keeps creeping up.
Why does metabolic syndrome raise blood pressure? It’s tied to insulin resistance and inflammation. Excess fat makes your blood vessels stiff. Your kidneys hold onto more sodium and water. Your sympathetic nervous system gets overactive. All of this forces your heart to work harder, pushing pressure through your arteries.
Even if you’re on medication for blood pressure, having metabolic syndrome means your treatment needs to be smarter. Just lowering the number isn’t enough. You have to fix the root cause-or the problem will come back.
Lipid Chaos: Triglycerides Up, HDL Down
Your blood fats tell a story. Triglycerides are your body’s way of storing extra energy. When you eat too many refined carbs and sugars, your liver turns them into triglycerides and floods your bloodstream. Levels above 150 mg/dL are a red flag.
Meanwhile, HDL cholesterol-your "good" cholesterol-is supposed to sweep up excess fat and take it back to the liver. But in metabolic syndrome, HDL drops below 40 mg/dL in men and 50 mg/dL in women. Why? Because insulin resistance messes with the enzymes that make HDL. It’s like your body’s cleanup crew has been laid off.
This combo-high triglycerides and low HDL-is one of the strongest predictors of plaque buildup in your arteries. It’s not just about cholesterol numbers. It’s about the *type* of particles. Metabolic syndrome makes your LDL cholesterol smaller and denser. These tiny particles slip into artery walls more easily and cause more damage.

Why You Don’t Feel It Until It’s Too Late
Metabolic syndrome is quiet. That’s why it’s so dangerous. You might have all five risk factors and still feel fine. No chest pain. No fatigue. No blurred vision. The only obvious sign? A waistline that won’t shrink.
Some people notice subtle clues: feeling foggy after meals, needing to urinate more often, or getting tired easily. But these are often dismissed as "just aging" or "stress." The truth? They’re early signals your body is struggling to manage sugar and fat.
And here’s something most don’t realize: metabolic syndrome doesn’t just hurt your heart. It’s linked to fatty liver disease, sleep apnea, polycystic ovary syndrome (PCOS), and even some types of cancer. The inflammation that drives metabolic syndrome doesn’t stop at your blood vessels. It spreads.
Who’s Most at Risk?
Age is a big factor. About 20% of people in their 20s and 30s have metabolic syndrome. By 60, that number nearly doubles. But it’s not just about getting older.
People with these traits are at higher risk:
- Abdominal obesity, even if overall weight is normal
- Family history of type 2 diabetes or heart disease
- Physical inactivity-sitting more than 8 hours a day
- Diets high in sugary drinks, white bread, pastries, and fried foods
- Ethnicity: African Americans, Hispanics, Native Americans, and South Asians have higher rates
- Women with PCOS
- History of gestational diabetes
And here’s the surprise: you don’t have to be overweight. Some people with "normal" BMI still have visceral fat and insulin resistance. That’s called "TOFI"-thin on the outside, fat inside. It’s more common than you think.
The Only Proven Treatment: Lifestyle, Not Pills
There’s no magic pill for metabolic syndrome. Drugs can help manage blood pressure, cholesterol, or blood sugar-but they don’t fix the core problem. Only lifestyle changes do.
The most powerful intervention? Losing 5 to 10% of your body weight. That’s not about becoming thin. It’s about losing enough fat to reset your metabolism. For someone who weighs 200 pounds, that’s just 10 to 20 pounds. And the results? Studies show:
- Triglycerides drop by 20-30%
- HDL increases by 10-15%
- Blood pressure falls by 5-10 mmHg
- Fasting blood sugar normalizes in up to 60% of cases
How? Two things: movement and food.
Move more. Aim for 150 minutes a week of brisk walking, cycling, or swimming. That’s 30 minutes, five days a week. Strength training twice a week helps too-muscle burns sugar better than fat.
Eat differently. Cut out sugary drinks, white bread, and processed snacks. Focus on vegetables, whole grains, legumes, nuts, fish, and lean proteins. Olive oil over butter. Water over soda. Real food over packaged stuff.
One study from Penn Medicine tracked 200 people with metabolic syndrome over 12 months. Those who followed a structured diet and exercise plan had a 65% success rate in reversing the syndrome. No drugs. Just food and movement.

What About Medications?
Medications are tools, not solutions. If your blood pressure is dangerously high, you’ll need a pill. If your cholesterol is out of control, statins may help. If your blood sugar is creeping up, metformin can delay diabetes.
But here’s the catch: if you don’t change your lifestyle, the drugs will only mask the problem. And you’ll likely need more of them over time.
The best approach? Treat each piece individually, but focus on the whole. A doctor might prescribe a statin for your cholesterol, an ACE inhibitor for your blood pressure, and metformin for your blood sugar. But unless you lose the belly fat, the cycle continues.
Can You Reverse It?
Yes. And not just slow it down-reverse it.
Research from the Cleveland Clinic and Framingham Heart Study shows that people who lose weight, move regularly, and eat well can completely undo metabolic syndrome. It doesn’t happen overnight. But within 6 to 12 months, many see all five markers return to normal.
It’s not about perfection. It’s about consistency. One day of pizza won’t ruin it. But three days a week of fast food? That keeps the fire burning.
The key is catching it early. If you’re over 40, have a waist over 35 inches (women) or 40 inches (men), and your last blood test showed high triglycerides or low HDL-don’t wait for a doctor to say something’s wrong. Start now.
What Should You Do Next?
Take action. Here’s your simple plan:
- Measure your waist. If you’re above the cutoff, you’re at risk.
- Check your last blood test. Look for triglycerides ≥150, HDL below 40 (men) or 50 (women), fasting glucose ≥100.
- Get your blood pressure checked. If it’s 130/85 or higher, it’s a red flag.
- Start walking 30 minutes a day, five days a week.
- Replace one sugary drink with water every day.
- Schedule a visit with your doctor. Ask for a full metabolic panel.
You don’t need a fancy program. You don’t need to join a gym. You just need to start moving and eating better. The science is clear: metabolic syndrome isn’t a life sentence. It’s a signal. And you have the power to change it.

 Medications
Medications
laura Drever
January 12, 2026 AT 16:40James Castner
January 13, 2026 AT 03:57lucy cooke
January 14, 2026 AT 18:00Clay .Haeber
January 16, 2026 AT 09:05Priyanka Kumari
January 17, 2026 AT 00:04Vinaypriy Wane
January 17, 2026 AT 17:34Diana Campos Ortiz
January 19, 2026 AT 09:06Jesse Ibarra
January 19, 2026 AT 13:30Acacia Hendrix
January 21, 2026 AT 07:03Adam Rivera
January 22, 2026 AT 19:15sam abas
January 23, 2026 AT 02:22Kimberly Mitchell
January 24, 2026 AT 22:38Robin Williams
January 25, 2026 AT 08:42Trevor Davis
January 25, 2026 AT 22:57