When you have G6PD deficiency, even a common pill can trigger a dangerous drop in red blood cells. This isn’t theoretical-it happens in hospitals every day. A 42-year-old man in Ohio was given methylene blue for methemoglobinemia without being tested for G6PD deficiency. Within 48 hours, his hemoglobin plunged from 14.2 g/dL to 5.8 g/dL. He needed three units of blood. This isn’t rare. In fact, 68% of people with G6PD deficiency report at least one hemolytic episode, often because their doctor didn’t know the risks.
What Is G6PD Deficiency?
G6PD deficiency is a genetic condition that affects how your red blood cells handle stress. The enzyme glucose-6-phosphate dehydrogenase helps protect those cells from damage caused by oxidative stress. When this enzyme doesn’t work properly, your red blood cells break down too easily-especially when exposed to certain drugs, foods, or infections. It’s not something you can outgrow. It’s not curable. But it’s completely preventable-if you know what to avoid.
It’s most common in people with ancestry from Africa, the Mediterranean, Southeast Asia, and the Middle East. In some parts of sub-Saharan Africa, one in five people carries the gene. In the U.S., about 1 in 10 African American males has it. Many people never know they have it until they’re given a dangerous medication-or until their child is born with jaundice that won’t go away.
Why Certain Medications Are Dangerous
Not all drugs are risky. But about 87 medications on the WHO’s Essential Medicines List can cause hemolysis in people with G6PD deficiency. These aren’t obscure drugs-they’re commonly prescribed.
- Rasburicase-used to treat tumor lysis syndrome. The FDA has a black box warning: it causes 100% hemolysis in deficient patients. One case reported in the American Journal of Emergency Medicine involved a 28-year-old who received rasburicase without testing. His hemoglobin dropped to 3.1 g/dL. He needed 10 units of blood.
- Methylene blue-used for methemoglobinemia. In G6PD-deficient patients, it causes severe hemolysis in 95% of cases. It’s ironic: a drug meant to fix oxygen delivery in the blood can destroy red blood cells in people with this deficiency.
- Primaquine-used to treat malaria. For people with Class I or II G6PD deficiency, it’s deadly. WHO guidelines now require testing before use. In Thailand, after making G6PD testing mandatory before primaquine, hemolytic crises dropped from 15.2% to 0.3%.
- Dapsone-used for leprosy and some skin conditions. At doses above 50mg daily, it causes hemolysis in 80% of deficient patients.
Even drugs you might assume are safe can be risky. Sulfonylureas like glyburide (used for diabetes) carry warnings on their labels, but the evidence is weak-only 17 cases ever documented since 1965. Yet, 92% of their packaging still includes the warning. This creates confusion and unnecessary fear.
Safe Alternatives
The good news? You don’t have to go without treatment. There are safe alternatives for almost every risky drug.
- For malaria prevention: Use atovaquone-proguanil (Malarone) instead of primaquine. A 2021 study of 1,245 travelers with G6PD deficiency showed 95% avoided hemolysis using this combo.
- For malaria treatment: Artemisinin-based combination therapies (like artemether-lumefantrine) are safe in all G6PD deficiency classes.
- For methemoglobinemia: Instead of methylene blue, use ascorbic acid (vitamin C) or exchange transfusion if severe.
- For tumor lysis syndrome: Use allopurinol instead of rasburicase. It’s slower but safe.
- For pain relief: Avoid aspirin and high-dose acetaminophen. Stick to low-dose acetaminophen or ibuprofen-both are generally safe at standard doses.
One of the biggest breakthroughs is tafenoquine, a new drug approved in 2018 for radical cure of malaria. It’s more effective than primaquine-but only if you’ve been tested for G6PD deficiency first. The FDA requires testing before prescribing it. This is a model for how drug safety should work.

Testing Is Not Optional
Many people think G6PD deficiency only affects men. It doesn’t. About 15% of women with the gene can still have hemolysis due to how X-chromosome inactivation works. So if your mother had jaundice as a baby, or your uncle had a bad reaction to a drug, you could be at risk.
Testing is simple. The fluorescent spot test gives results in 15 minutes. It’s 98.7% accurate. In Saudi Arabia, after making newborn screening mandatory, hospital admissions for hemolytic crises dropped by 78% between 2010 and 2020.
But here’s the catch: you can’t test during or right after a hemolytic episode. Your red blood cells are young and still have enough enzyme to mask the deficiency. You need to wait at least three months after an episode for an accurate result. If you’ve had unexplained anemia after taking a drug, get tested after the recovery period.
What to Do If You’ve Never Been Tested
If you’re from a high-risk region, or you’ve had unexplained jaundice, dark urine after taking a drug, or a family history of anemia, get tested. Don’t wait for a crisis.
Here’s your checklist:
- Ask your doctor for a G6PD test-especially if you’re planning surgery, pregnancy, or travel to a malaria-endemic area.
- If you’re pregnant, get tested before taking any new medication. Your baby may inherit the deficiency.
- Keep a list of unsafe drugs and show it to every new provider. Print it out. Put it in your wallet.
- Wear a medical alert bracelet that says “G6PD Deficient.”
- Ask for a copy of your test results. Don’t rely on old charts or memory.
People who get proper education and avoid triggers have a 92% chance of never having a hemolytic episode. Those who don’t? 62% will have at least one by age 40.
What About Fava Beans and Infections?
Yes, fava beans can trigger hemolysis. That’s why it’s sometimes called “favism.” But not everyone with G6PD deficiency reacts to them. It depends on the variant. Mediterranean variants are more sensitive. African variants less so.
Infections-like pneumonia or the flu-can also trigger hemolysis. That’s because they create oxidative stress. If you’re sick and you have G6PD deficiency, avoid NSAIDs like ibuprofen unless approved by your doctor. Stick to acetaminophen. Stay hydrated. Monitor for dark urine or fatigue.
Future Hope
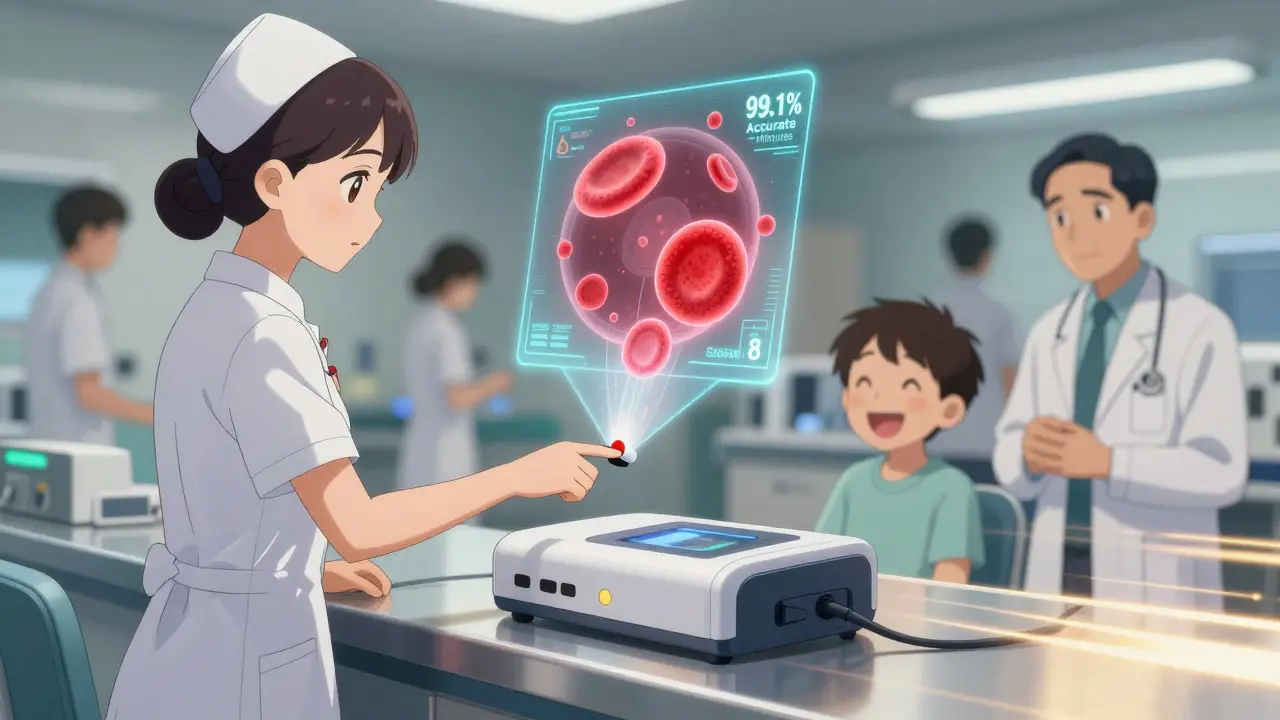
There’s progress. In January 2024, the FDA approved the first point-of-care G6PD test that gives results in 8 minutes with 99.1% accuracy. That’s huge for emergency rooms and clinics without labs.
Researchers are also testing N-acetylcysteine (NAC), a common antioxidant, to protect red blood cells during exposure to risky drugs. Early lab results show it reduces hemolysis by 75% when given with primaquine.
By 2035, experts believe preventable deaths from G6PD deficiency could be nearly eliminated in countries with good healthcare. But right now, 85% of deaths happen in places without testing programs. That’s not a medical problem-it’s a systems problem.
Final Thought: Knowledge Saves Lives
G6PD deficiency isn’t a death sentence. It’s a condition you manage with awareness. The drugs aren’t evil. The condition isn’t rare. The problem is silence. Too many people don’t know they have it. Too many doctors don’t ask. Too many patients don’t speak up.
If you’ve ever had dark urine after taking a pill, or if your child had jaundice that didn’t go away, get tested. If you’re prescribed a new drug, ask: “Is this safe for G6PD deficiency?” Don’t assume it is. Write it down. Keep a list. Tell your pharmacist. Your life might depend on it.
Can G6PD deficiency be cured?
No, G6PD deficiency is a genetic condition and cannot be cured. But it can be effectively managed by avoiding oxidative stressors like certain medications, fava beans, and infections. With proper precautions, people with G6PD deficiency live normal, healthy lives.
Is G6PD deficiency only a problem for men?
No. While it’s more common in men because the gene is on the X chromosome, women can also be affected. About 15% of women who carry the gene experience hemolysis due to random X-chromosome inactivation. This means some of their red blood cells lack the enzyme, making them vulnerable to oxidative damage.
What should I do if I accidentally take a dangerous medication?
Stop taking the medication immediately. Seek medical help right away. Symptoms of hemolysis include dark urine, extreme fatigue, yellowing skin, rapid heartbeat, and shortness of breath. Blood tests will check your hemoglobin and reticulocyte count. Treatment may include fluids, oxygen, and in severe cases, a blood transfusion. The sooner you act, the better the outcome.
Can I get G6PD testing done at my local pharmacy?
In many places, yes. Point-of-care G6PD tests are now available in some pharmacies and clinics, especially in regions with high prevalence. The new STANDARD G6PD Test System gives results in 8 minutes and is approved for use in emergency settings. Ask your doctor or pharmacist if they offer rapid testing.
Are herbal supplements safe for people with G6PD deficiency?
Many are not. Supplements like naphthalene (mothballs), vitamin K3, and certain Chinese herbs (e.g., dan shen) can trigger hemolysis. Even natural products like tea tree oil or high-dose vitamin C can be risky. Always check with your doctor before taking any supplement, even if it’s labeled “natural” or “herbal.”
How often should I get retested for G6PD deficiency?
Once is usually enough. G6PD deficiency is genetic and doesn’t change over time. However, if you had a recent hemolytic episode, wait at least three months before testing for accurate results. Newborns who test positive should be reconfirmed in infancy if the initial test was borderline.
Can I donate blood if I have G6PD deficiency?
Yes, you can donate blood as long as you’re not currently in a hemolytic episode. However, your blood may be flagged for G6PD status, and it may not be used for transfusions in patients with the same deficiency. Always inform the blood bank about your condition when you donate.


 Medications
Medications
Nadia Watson
January 21, 2026 AT 11:29It’s staggering how often this gets overlooked. I work in a hospital in Ohio, and I’ve seen it happen twice in the last year alone. One patient came in with severe anemia after taking a simple antibiotic for a UTI. No one asked about family history or ancestry. No one thought to test. It’s not just about prescribing-it’s about systemic ignorance. We need mandatory screening in high-risk populations before any non-urgent medication is given. This isn’t rare. It’s preventable. And we’re failing.
Courtney Carra
January 22, 2026 AT 01:26It’s wild how medicine still treats genetic conditions like they’re optional disclosures. 🤔 Like, if you’re gonna give someone a drug that can kill them, maybe ask if they’re from a region where 1 in 5 people carry this? But nope. We’d rather wait for someone to turn purple and need 10 units of blood before we ‘consider’ it. The fact that we have point-of-care tests now and still don’t use them? That’s not negligence. That’s choice.
thomas wall
January 23, 2026 AT 07:51This post is a textbook example of medical malpractice by omission. The fact that such a widespread, well-documented genetic condition remains undiagnosed in the majority of affected individuals is not merely a failure of awareness-it is a moral failing of the medical establishment. Every physician who prescribes primaquine, methylene blue, or rasburicase without testing is, in effect, gambling with human life. There is no excuse. No ‘overcaution.’ No ‘rare incidence.’ When the data is this clear, inaction is complicity.
Paul Barnes
January 25, 2026 AT 06:14Correct me if I’m wrong, but the FDA black box warning for rasburicase has been around since 2004. So why are we still seeing cases? Because doctors don’t read labels. Or they assume someone else tested. Or they think ‘it won’t happen to me.’ This isn’t a knowledge gap. It’s a compliance gap. And it’s killing people.
sagar sanadi
January 26, 2026 AT 12:20Wait so you’re telling me if you’re brown and get a fever, you can’t take ibuprofen? That’s racist. They made this up so white doctors feel smart. Next they’ll say we can’t eat beans because we’re ‘genetically prone’ to something. This is just pharma fear-mongering to sell more tests.
kumar kc
January 27, 2026 AT 09:26Testing should be free and mandatory at birth. No excuses. End of story.
Carolyn Rose Meszaros
January 28, 2026 AT 02:22I’m a nurse and I’ve had two patients with G6PD deficiency who didn’t know they had it. One was my cousin. She had jaundice as a baby, but no one ever followed up. Now she’s terrified of every new medication. I printed out the safe/unsafe list and laminated it for her. It’s not complicated. Just ask. Just test. It takes 15 minutes. Lives are on the line. 💔
Greg Robertson
January 28, 2026 AT 04:58Just had this conversation with my doctor last week. I’m African American, had a cousin die young from an ‘unknown’ anemia. I asked about G6PD testing before my knee surgery. He said, ‘Oh, we don’t usually test unless someone’s from Africa or Asia.’ I told him I was born in Detroit. He paused. Then he ordered the test. It came back positive. I’m so glad I spoke up. This stuff matters.
Jacob Cathro
January 29, 2026 AT 04:59So let me get this straight. If you’re black or brown or from India, you can’t take ibuprofen or malaria meds without a blood test? But if you’re white, you can just pop pills like candy? And now they want us to wear medical bracelets like we’re radioactive? This isn’t medicine. This is genetic profiling dressed up as safety. Who’s really benefiting here? Pharma? Labs? Or are we just being turned into walking risk assessments?