High Blood Pressure – What You Need to Know
When talking about high blood pressure, a condition where the force of blood against artery walls stays higher than normal. Also known as hypertension, it raises the risk of heart attacks, strokes, and kidney problems. Understanding it is the first step toward keeping your arteries healthy.
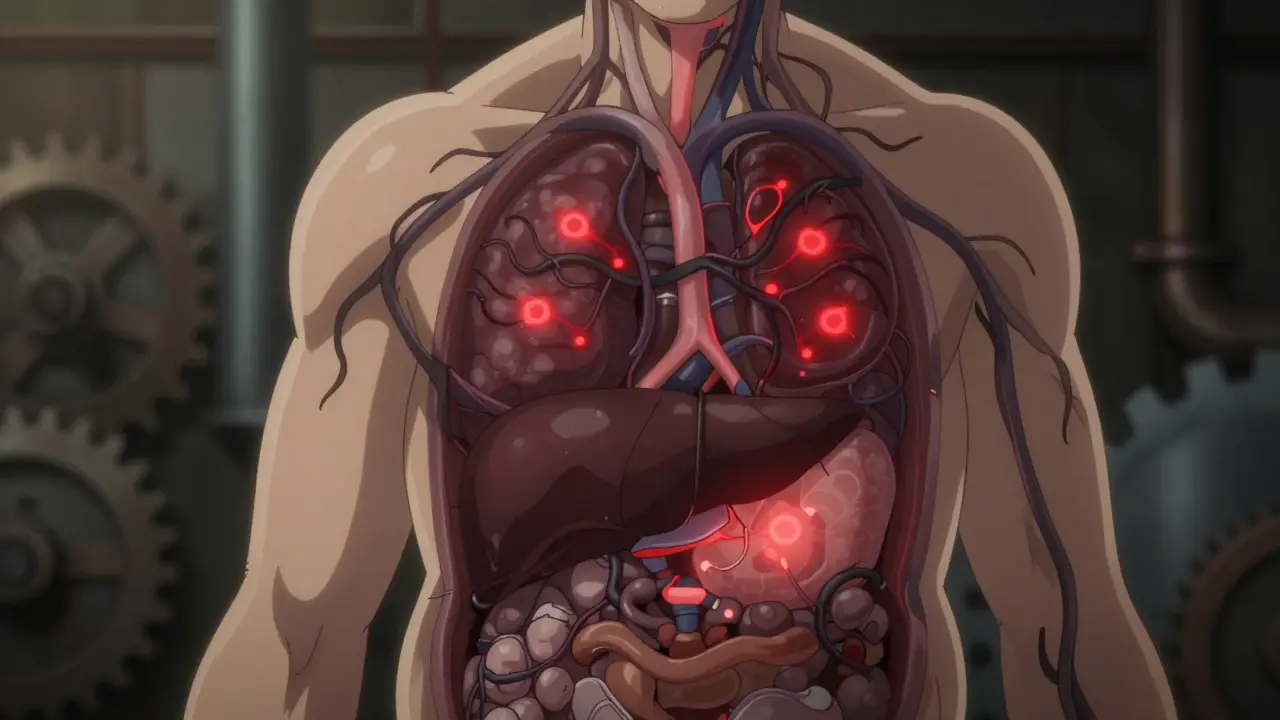
High blood pressure doesn’t exist in a vacuum; it’s a major player in cardiovascular disease, a group of disorders that affect the heart and blood vessels. Cardiovascular disease includes conditions like coronary artery disease, heart failure, and peripheral artery disease, all of which share the common thread of impaired blood flow. When your pressure stays high, the extra strain can damage arterial walls, making plaque buildup easier and leading to blockages. In short, high blood pressure fuels cardiovascular disease, and managing one helps control the other.
Why Lifestyle Changes Matter
One of the most powerful ways to tackle high blood pressure is through lifestyle modification, which covers diet, exercise, stress management, and sleep quality. Research shows that cutting sodium, adding potassium‑rich foods, and adopting the DASH diet can lower systolic numbers by up to 10 mmHg. Regular aerobic activity—like brisk walking, cycling, or swimming—helps vessels stay flexible and improves heart efficiency. Stress reduction techniques such as mindfulness or yoga also play a role because chronic stress triggers hormone spikes that tighten blood vessels. In other words, high blood pressure requires lifestyle modifications to give medication a better chance of working.
Another key factor is maintaining a healthy weight. Even a modest loss of 5‑10 % of body weight can translate into a noticeable drop in pressure. Smoking cessation is non‑negotiable; each cigarette raises artery stiffness, pushing readings higher. Lastly, limiting alcohol to moderate levels (no more than two drinks per day for men, one for women) keeps the heart from over‑working.
Beyond habits, many people rely on antihypertensive medication, which includes classes like ACE inhibitors, beta‑blockers, calcium channel blockers, and diuretics. These drugs target different pathways—some relax blood vessels, others reduce fluid volume, and a few lower heart rate. Choosing the right combo often depends on age, kidney function, and any co‑existing conditions, such as diabetes or chronic kidney disease. Regular check‑ups are crucial because dosage adjustments may be needed as your body responds. In short, antihypertensive medication influences blood pressure control and works best when paired with lifestyle changes.
Accurate self‑monitoring rounds out the management plan. Home blood pressure cuffs let you track trends, spot white‑coat spikes, and share data with your doctor. Aim for two readings each morning and evening, and record them for at least a week before any medication changes. Consistency helps you see what works—whether it’s a new diet, a new exercise routine, or a medication tweak.
All of these pieces—understanding the condition, addressing its link to cardiovascular disease, adopting lifestyle modifications, using medication wisely, and monitoring regularly—create a comprehensive approach. Below you’ll find a curated list of articles that dive deeper into each of these areas, from exercise plans for vascular health to comparisons of heart‑supporting herbs and the latest medication guides. Keep reading to get practical tips you can apply right away and stay ahead of the risks that high blood pressure brings.
Metabolic syndrome is a cluster of conditions-abdominal obesity, high blood pressure, and abnormal lipids-that raise your risk of heart disease and diabetes. Learn what it means, who’s at risk, and how to reverse it with lifestyle changes.
Discover how Olmesartan lowers blood pressure, its benefits over ACE inhibitors, safety profile, and practical tips for optimal hypertension management.

 Medications
Medications