Medication Side Effects Checker
This tool helps you understand potential sexual side effects of common medications based on medical research. It does NOT replace professional medical advice.
Important: Always discuss medication changes with your doctor. Never stop or change medications without professional guidance.
Which medications are you taking?
Select all that apply
Your Results
Next Steps
- Discuss with your doctor: "Could my medication be affecting my sex life?"
- Ask about safer alternatives if appropriate
- Consider timing adjustments (e.g., taking SSRIs after sex)
- Try non-pharmacological approaches like exercise
It’s not uncommon to feel embarrassed talking about sex-especially when it’s not going as it should. But if you’ve noticed a drop in desire, trouble getting or keeping an erection, or difficulty reaching orgasm, and you’re on medication, you’re not alone. In fact, sexual side effects from common medications are one of the most underdiscussed, yet widespread, problems in modern medicine. Studies show that up to 73% of people taking certain antidepressants experience sexual problems. That’s more than two out of every three patients. And it’s not just antidepressants. Blood pressure pills, heart meds, even acid reflux drugs can quietly sabotage your sex life. The good news? You don’t have to just accept it. There are real, practical ways to manage this-and you don’t need to suffer in silence.
Antidepressants Are the Biggest Culprit
If you’re on an SSRI-like sertraline (Zoloft), fluoxetine (Prozac), or paroxetine (Paxil)-you’re at high risk. These drugs work by boosting serotonin, which helps lift mood. But serotonin also puts the brakes on sexual response. The result? Lower libido, delayed or absent orgasm, and sometimes even erectile issues. Paroxetine carries the highest risk: about 65% of users report sexual side effects. Fluvoxamine and sertraline aren’t far behind, with rates around 59% and 56% respectively. Even if your depression improves, these side effects can make you feel worse emotionally-because sex is tied to intimacy, confidence, and self-worth.Not all antidepressants are the same, though. Bupropion (Wellbutrin) and mirtazapine (Remeron) are known for having much lower rates of sexual side effects. In fact, some people report improved libido on bupropion. If sexual function matters to you-and it should-this isn’t just a side note. It’s a key factor in choosing the right medication. Talk to your doctor about switching. Don’t stop cold turkey. Withdrawal from SSRIs can cause dizziness, nausea, or even brain zaps. But with careful planning, many people successfully transition to a better-tolerated option.
Heart and Blood Pressure Medications Can Slow Things Down
High blood pressure isn’t just a heart issue-it’s a sexual one too. Many of the drugs used to treat it reduce blood flow, which directly affects arousal and erection. Thiazide diuretics like hydrochlorothiazide (Microzide) are the most likely to cause erectile dysfunction among antihypertensives. Beta blockers like atenolol are next. Both reduce the body’s ability to pump blood to the genitals, which makes arousal harder.But here’s something surprising: not all blood pressure meds have the same effect. Angiotensin II receptor blockers like valsartan have actually been linked to improved sexual desire in women, compared to beta blockers. If you’re a woman on blood pressure meds and notice you’re less interested in sex or don’t enjoy it as much, it could be the drug-not your relationship or your age. About 41% of women on these medications report lower desire. For men, the numbers are just as striking: up to 10% of heart failure patients say their sexual problems started after starting meds like digoxin or spironolactone.
Before you blame yourself or your partner, ask your doctor if your blood pressure pill could be the cause. Sometimes, switching to a different class of medication-like an ARB or ACE inhibitor-can make a big difference without sacrificing blood pressure control.
Prostate Medications and Antiandrogens: A Trade-Off
Men taking finasteride (Propecia, Proscar) or dutasteride for hair loss or enlarged prostate may notice a drop in libido or trouble ejaculating. These drugs block DHT, a hormone that affects both hair follicles and sexual function. Studies show 5.9% to 15.8% of users report lower desire, and 5.1% to 9% develop erectile dysfunction. For many, the trade-off feels worth it for hair retention-but if sex is important to you, this isn’t a minor side effect. It’s life-changing.For men with prostate cancer, antiandrogens like bicalutamide are used to shut down testosterone. Almost all men on these drugs lose libido, develop erectile dysfunction, and may even get breast tissue growth (gynecomastia). These effects are expected. But that doesn’t mean they’re easy to live with. That’s why counseling before starting treatment is critical. Knowing what’s coming helps men prepare emotionally and practically. Some couples use this time to explore new ways of being intimate-touch, closeness, non-penetrative pleasure-that don’t rely on erection or orgasm.
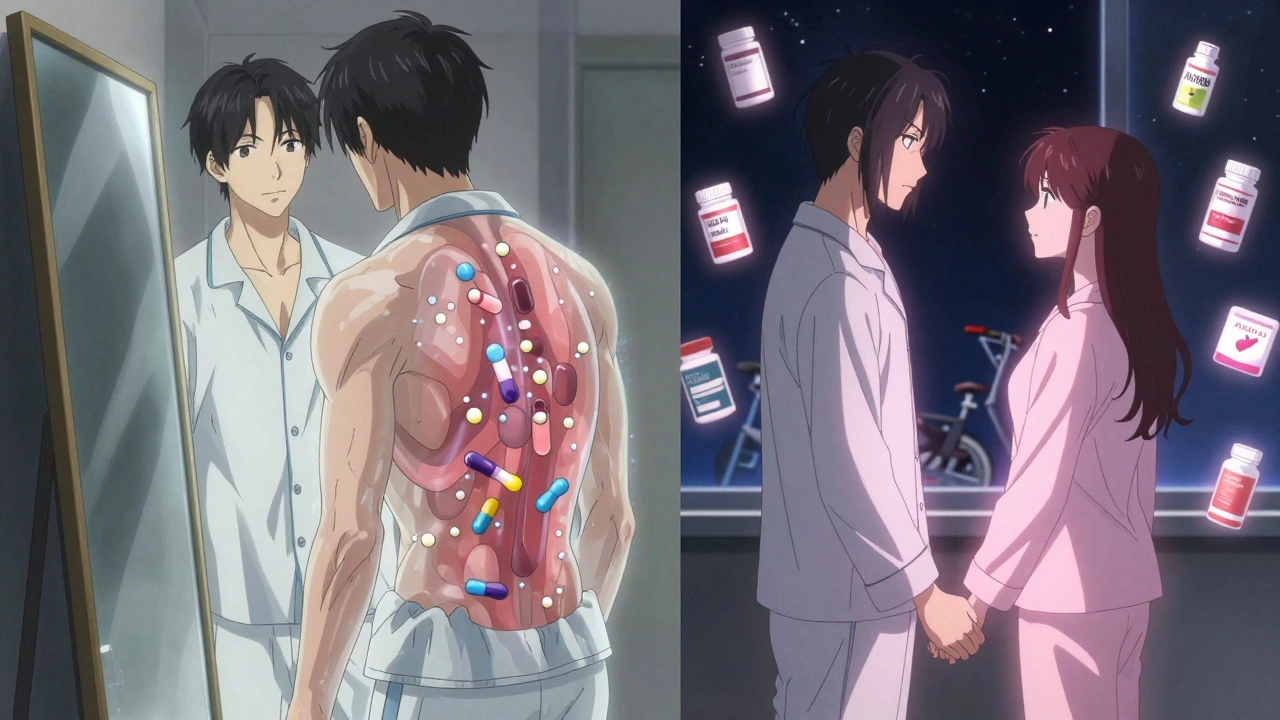
Other Surprising Offenders
You might not think of pain meds or acid reflux drugs as sexual killers-but they can be. Opioids like oxycodone and hydrocodone suppress testosterone by messing with the brain’s hormone signals. Long-term use can lead to secondary hypogonadism: low testosterone caused by the drug, not aging. That means low libido, fatigue, and even muscle loss-not because you’re getting older, but because your body’s hormone production got turned down.Antiepileptic drugs like gabapentin and pregabalin are also linked to sexual dysfunction. They raise a protein called sex hormone binding globulin, which locks up testosterone and makes it less available. Even though these drugs aren’t meant for sex, they can still mess with it.
And yes, proton pump inhibitors (PPIs) like omeprazole and H2 blockers like ranitidine have been tied to lower libido and erectile problems in some patients. The exact reason isn’t clear, but it’s happening often enough that doctors are starting to ask about it.
What You Can Do About It
The first step? Don’t assume it’s normal. Just because it’s common doesn’t mean it’s unavoidable. Here’s what actually works:- Talk to your prescriber. Bring up sexual side effects the same way you would talk about dizziness or dry mouth. They’ve heard it before. They can help.
- Consider switching. If you’re on paroxetine and struggling, ask about sertraline-or better yet, bupropion. If you’re on a thiazide diuretic, ask about an ARB like valsartan.
- Try a drug holiday. Under medical supervision, some people take a short break from SSRIs on weekends to allow sexual function to recover. This isn’t for everyone, but it works for some.
- Timing matters. Taking your SSRI after sex instead of before can reduce interference with arousal and orgasm.
- Add a helper. For men with SSRI-induced erectile dysfunction, sildenafil (Viagra) has been shown to help in 74-95% of cases. It’s not a cure for the root cause, but it can restore function while you work on longer-term solutions.
- Move your body. Regular exercise improves blood flow, boosts testosterone, and reduces stress-all of which help sexual function. Even 30 minutes of brisk walking five days a week can make a difference.
Why This Isn’t Just a ‘Man Problem’
Most of the research focuses on men-because erectile dysfunction is easier to measure. But women experience sexual side effects too, and they’re often ignored. Women on SSRIs report reduced desire, difficulty with arousal, and inability to orgasm. On antihypertensives, 34% report less sexual pleasure. These aren’t minor complaints. They affect relationships, self-esteem, and mental health.And here’s the kicker: depression itself can cause sexual dysfunction. Up to 70% of people with depression have low libido-even before taking meds. That’s why it’s so hard to tell if the problem is the illness or the treatment. That’s why open, honest conversations with your doctor are so important. You need to know: Is this the depression? The drug? Or both?
What’s Changing in the Field
The medical world is waking up. The FDA now requires drug makers to report sexual side effects in clinical trials for CNS medications. The American Urological Association recommends routine screening for sexual dysfunction in patients on long-term antidepressants, blood pressure meds, or prostate drugs. Researchers are developing new antidepressants that don’t spike serotonin as much-and therefore don’t crush libido. Some are even testing drugs that boost dopamine or norepinephrine, which can actually improve sexual function.For now, the best tool you have is awareness. If you’re on medication and your sex life has changed, it’s not your fault. It’s not weakness. It’s pharmacology. And it’s fixable.
Can antidepressants permanently affect sexual function?
In most cases, sexual side effects from antidepressants are reversible once the medication is stopped or changed. However, a small number of people report persistent symptoms-called Post-SSRI Sexual Dysfunction (PSSD)-even after discontinuing the drug. While rare, this condition is documented in medical literature and can last months or longer. If you experience ongoing issues after stopping an SSRI, see a specialist. There’s no standard treatment yet, but some find relief with bupropion, hormone testing, or counseling.
Is it safe to take Viagra with antidepressants?
Yes, sildenafil (Viagra) is generally safe to take with SSRIs, and it’s often prescribed specifically for SSRI-induced erectile dysfunction. Studies show it helps in 74-95% of cases. But you still need to talk to your doctor. Combining medications can sometimes affect blood pressure or cause dizziness. Your doctor will check for interactions and make sure the dose is right for you.
Do all blood pressure meds cause sexual problems?
No. Thiazide diuretics and beta blockers are the most likely to cause issues. But angiotensin II receptor blockers (like valsartan) and ACE inhibitors (like lisinopril) have much lower rates of sexual side effects-and in some studies, women on ARBs actually reported improved sexual desire compared to those on beta blockers. If you’re on a high-risk medication, ask if switching is an option.
Can I just stop my medication if sex is affected?
Never stop medication abruptly. Stopping SSRIs suddenly can cause withdrawal symptoms like dizziness, nausea, anxiety, or electric-shock sensations. Stopping blood pressure meds can spike your blood pressure dangerously. Always work with your doctor. They can help you taper safely or switch to a better-tolerated drug.
Are there natural ways to counteract these side effects?
Exercise is the most proven natural method-it improves blood flow, boosts testosterone, and reduces stress. Some people find that reducing alcohol, quitting smoking, and managing stress help too. Supplements like L-arginine or ginseng are sometimes tried, but there’s limited evidence they work for drug-induced dysfunction. Always talk to your doctor before starting supplements, especially if you’re on heart or blood pressure meds.
Why isn’t this talked about more in doctor’s offices?
Many doctors assume patients won’t bring it up-or that it’s too embarrassing. But studies show that when doctors ask directly, patients are more likely to talk about it. If your doctor doesn’t bring it up, you should. You’re not being awkward-you’re being proactive. Sexual health is part of your overall health. If your doctor dismisses it, it’s time to find one who takes it seriously.


 Medications
Medications
Chad Kennedy
December 3, 2025 AT 09:56Siddharth Notani
December 4, 2025 AT 03:24Cyndy Gregoria
December 4, 2025 AT 05:52Akash Sharma
December 4, 2025 AT 06:44Justin Hampton
December 5, 2025 AT 02:00Chris Jahmil Ignacio
December 6, 2025 AT 22:37Paul Corcoran
December 7, 2025 AT 17:29Colin Mitchell
December 8, 2025 AT 10:13Stacy Natanielle
December 8, 2025 AT 20:37kelly mckeown
December 10, 2025 AT 10:26Tom Costello
December 11, 2025 AT 23:35dylan dowsett
December 12, 2025 AT 22:40