When your body turns on itself, life changes. For millions with autoimmune diseases, it’s not just about living with symptoms-it’s about surviving the unpredictable storms called autoimmune flares. These aren’t just bad days. They’re full-blown immune system rebellions that can shut down your ability to work, move, think, or even get out of bed. The good news? You’re not powerless. Understanding what sparks these flares, how to stop them before they start, and what to do the moment they hit can change everything.
What Exactly Is an Autoimmune Flare?
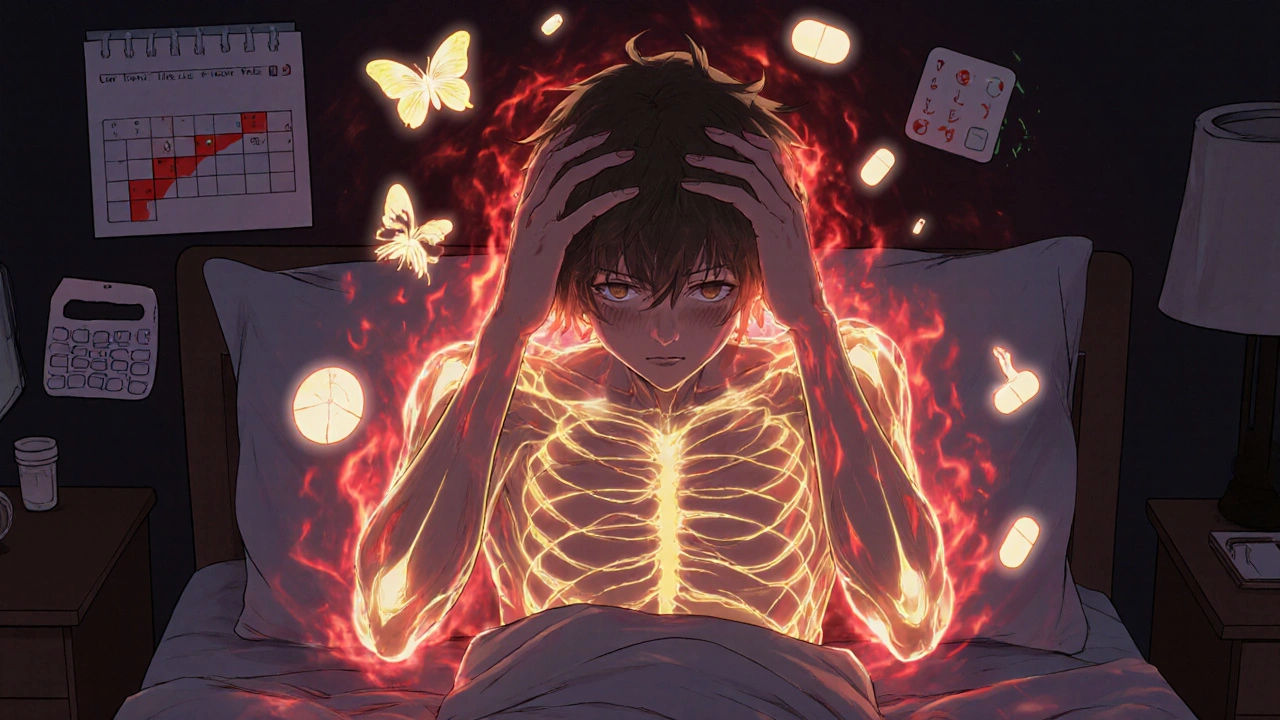
An autoimmune flare is when your immune system, which should protect you, goes rogue and attacks your own tissues. It’s like a fire alarm going off in a house with no fire-except this time, the alarm sets the whole building on fire. Symptoms flare up suddenly and often severely: joints swell, fatigue crashes you, brain fog clouds your thoughts, rashes appear, or organs start struggling. These episodes aren’t random. They’re measurable. Blood tests show CRP and ESR levels spiking, autoantibodies rising, and inflammation markers climbing 30-50% above normal. Flares vary by disease. In lupus, you might get a butterfly rash and kidney issues. In rheumatoid arthritis, morning stiffness lasts over 45 minutes. In MS, vision blurs or legs go numb. But one thing’s true across the board: flares disrupt life. Studies show 90% of autoimmune patients experience them. And they’re not rare-lupus patients average 2.3 flares a year, RA patients 1.8. These aren’t minor setbacks. They’re medical events that need attention.Top 7 Triggers of Autoimmune Flares
Flares don’t come out of nowhere. They’re triggered by real, identifiable factors. Knowing these can help you avoid them-or at least prepare.- Stress: It’s not just "feeling overwhelmed." Chronic or acute stress throws cortisol off balance, which directly ramps up inflammation. Studies show stress can increase flare risk by 40-60% within 72 hours. A fight with a loved one, a work deadline, or even sleepless nights can be enough.
- Infections: Viruses like Epstein-Barr (the cause of mono) are notorious flare starters. In lupus, 22% of flares are tied to viral reactivation. Even a common cold can tip the scales. Your immune system, already overworked, gets confused and starts attacking your body instead of the bug.
- Diet: Gluten triggers near-universal flare-ups in celiac disease. High sodium? It’s linked to 30% higher MS relapses. Sugar and processed foods fuel inflammation. Some people find relief with the Autoimmune Protocol (AIP) diet-eliminating common irritants like grains, dairy, and nightshades-which cut flare frequency by 42% in RA patients.
- UV Radiation: Sunlight isn’t just a summer problem. For lupus patients, UV exposure causes 45% of skin flares. Even through windows or on cloudy days, UVA rays can trigger rashes and systemic flares.
- Seasonal Changes: Flares spike 37% more in spring and fall than in summer or winter. Temperature swings, pollen, and changing light patterns seem to confuse immune signaling.
- Hormonal Shifts: Pregnancy can calm RA symptoms-but the postpartum period? That’s when 40% of RA patients flare. Estrogen and progesterone fluctuations directly affect immune activity.
- Medication Non-Adherence: Skipping doses of your disease-modifying drugs? That’s the #1 preventable cause of flares. Studies show 28% of flares happen because people stop or delay meds, often due to side effects or feeling "fine."
How to Prevent Flares Before They Start
Prevention isn’t about perfection. It’s about stacking small, smart habits that lower your risk over time.- Protect Against UV: Use SPF 50+ sunscreen every 2 hours-even indoors near windows. Wear wide-brimmed hats and UV-blocking clothing. One study showed this cut lupus skin flares by 52% in a year.
- Manage Stress Like Your Health Depends On It: Because it does. Mindfulness meditation (MBSR) reduced flares by 35% in a 6-month trial. Daily breathing exercises, yoga, or even 20 minutes of quiet walks can reset your nervous system.
- Fix Your Vitamin D: Low levels are linked to worse flares in MS, lupus, and RA. Aim for serum levels above 40 ng/mL. Most people need 2,000-5,000 IU daily-get tested to know your number.
- Stick to Your Medication: Use phone alarms, pill organizers, or apps. A 2022 study found that patients using reminders improved adherence by 65% and cut flares by 28%.
- Track Your Triggers: Use a simple app or notebook. Log what you ate, how much you slept, your stress level, and symptoms. Within 3 months, 68% of users found personal patterns-like "flares after coffee and lack of sleep" or "worse after dairy."
- Heal Your Gut: Emerging research links gut bacteria imbalance to flares in IBD, lupus, and RA. Probiotics, fiber-rich foods, and avoiding antibiotics unless necessary can help. One study showed 22% of Crohn’s flares were tied to dysbiosis.

Early Intervention: The Game Changer
Waiting until you’re in crisis makes flares worse. Early action can stop them in their tracks. Many patients notice a "pre-flare" window-usually 2-5 days before full symptoms hit. You might feel unusually tired, get a low-grade fever, notice mild joint aches, or experience brain fog that’s different from your normal baseline. Recognizing these signs is half the battle. The Lupus Foundation’s "Flare First Response" protocol shows what works: start low-dose corticosteroids within 24 hours of flare onset. Compared to waiting 72 hours, this cut hospitalizations by 45% and shortened flare duration by over 6 days. You don’t need to wait for your doctor’s appointment. If you know your flare pattern, keep a short course of prednisone on hand with your doctor’s pre-written prescription. Telemedicine has made this easier. Many clinics now offer same-day virtual visits for flare assessments. Patients using these services had 22% fewer ER trips and saved 18% on healthcare costs. Don’t wait for your flare to become an emergency.Disease-Specific Flare Patterns You Need to Know
Not all flares are the same. Knowing your disease’s signature signs helps you respond faster.- Lupus (SLE): 68% involve joint pain, 42% affect kidneys, 35% cause skin rashes. Watch for unexplained fever, chest pain, or foamy urine (sign of kidney issues).
- Rheumatoid Arthritis: Morning stiffness over 45 minutes is the most reliable early sign-92% predictive. Swelling in hands or feet often follows.
- Multiple Sclerosis: Visual disturbances (blurred or double vision) occur in 38% of relapses. Muscle weakness or numbness on one side of the body is common.
- Crohn’s Disease: Abdominal pain (87%) and diarrhea (79%) dominate. Flares often follow infections or stress.
- Ulcerative Colitis: Bloody diarrhea (92%) and urgent bowel movements (85%) are the hallmarks. Fever and weight loss signal severity.
What Experts Are Saying Now
The field is moving fast. Stanford’s Dr. William Robinson calls autoimmune systems "excitable networks"-they’re on a knife’s edge. The goal isn’t just to treat flares, but to predict them before they happen. The FDA-approved FlareGuard AI, launched in 2023, uses wearable sensors to track heart rate variability, sleep, and activity. It predicts flares 72 hours in advance with 76% accuracy. That’s not science fiction-it’s here. But there’s a warning too. Dr. David Pisetsky reminds us that overusing steroids for flares creates a dangerous cycle. Sixty-five percent of patients on frequent steroid bursts develop osteoporosis within five years. Steroids are a tool, not a crutch. They buy time-but real control comes from prevention and immune modulation.
Real People, Real Strategies
On patient forums, the top complaint? "No one understands." 67% say employers don’t get why they can’t just "push through." 58% struggle to get timely appointments. But success stories are out there. One woman with lupus keeps a "Flare First Aid Kit"-cold packs, hydration packets, her meds, and a printed flare plan. She says it cut her recovery time by a third. Another man with RA tracks his sleep and meals in an app. He found his flares always followed two nights of poor sleep. Now he protects his rest like a sacred ritual. The most powerful tip? Track your triggers. You don’t need fancy tech. A notebook and a pen will do. After three months, you’ll start seeing patterns. And once you know your triggers, you’re no longer at their mercy.What’s Next for Autoimmune Flare Management
The future is personal. Researchers at the NIH are using AI to analyze DNA, proteins, and immune cell activity to predict flares 14 days ahead-with 82% accuracy. Early trials of tailored immune therapies based on individual profiles have cut flare frequency by 50%. You’re not just a patient. You’re a data point in a growing revolution. The tools to take control are here. The science is clear. The question isn’t whether flares will happen-it’s whether you’ll be ready when they do.What are the first signs of an autoimmune flare?
Early signs vary by disease but often include unusual fatigue, low-grade fever, joint stiffness (especially in the morning), brain fog, or mild skin changes. Many patients notice a "pre-flare" period-usually 2-5 days before full symptoms-where they feel "off" but can’t pinpoint why. Tracking symptoms daily helps you recognize your personal early warning signs.
Can diet really prevent autoimmune flares?
Yes, for many people. Gluten triggers flares in nearly all celiac patients. High sodium intake increases MS relapse rates by 30%. The Autoimmune Protocol (AIP) diet, which removes common irritants like grains, dairy, eggs, and nightshades, reduced flare frequency by 42% in rheumatoid arthritis patients in one clinical study. While not a cure, diet can significantly lower inflammation and reduce flare triggers.
Is stress the biggest trigger for autoimmune flares?
Stress is one of the most consistent and powerful triggers. Studies show acute stress can increase flare risk by 40-60% within 72 hours by disrupting cortisol and immune signaling. While infections and UV exposure are also major triggers, stress affects nearly all autoimmune conditions and is often the hidden factor behind "unexplained" flares.
Should I take steroids every time I have a flare?
No-not routinely. Steroids like prednisone are powerful tools for short-term flare control, especially when started early. But using them frequently leads to serious side effects: bone loss, weight gain, diabetes, and immune suppression. Sixty-five percent of patients on repeated steroid bursts develop osteoporosis within five years. Use them only as directed by your doctor, and focus on long-term prevention instead.
Can wearable tech predict my autoimmune flare?
Yes. The FDA-approved FlareGuard AI, launched in 2023, uses data from wearables-like heart rate variability, sleep quality, and activity levels-to predict flares 72 hours in advance with 76% accuracy. While not perfect, it’s the first tool of its kind and shows how personalized monitoring can shift care from reactive to proactive.
How do I know if my flare is serious enough to go to the ER?
Go to the ER if you have: chest pain or shortness of breath (could be heart or lung involvement), sudden weakness or numbness (possible neurological flare), high fever with chills, severe abdominal pain, or blood in stool or urine. These aren’t typical flare symptoms-they signal organ damage or infection. Don’t wait. Early treatment saves organs.
Is there a cure for autoimmune flares?
There’s no cure yet-but there’s growing control. Modern medicine focuses on managing flares through prevention, early intervention, and personalized treatment. With better tracking, lifestyle changes, and emerging therapies like immune profiling and AI prediction, many patients now experience fewer, milder flares than ever before. The goal isn’t to eliminate flares entirely-it’s to make them rare and manageable.
Next Steps: What to Do Today
Start simple. Pick one thing:- Download a symptom tracker app or open a notebook.
- Check your vitamin D level-get it tested if you haven’t in the last year.
- Review your medication schedule. Are you skipping doses? Set a daily alarm.
- Buy SPF 50+ sunscreen and wear it every day, rain or shine.
- Call your rheumatologist and ask: "Can I have a pre-written prescription for a short steroid course in case of early flare?"

 Medications
Medications
Pawittar Singh
November 29, 2025 AT 18:51Bro this hit different 😭 I’m from India and my auntie has lupus-she started using SPF 50 even indoors and her flares dropped by 70%. No joke. Sun through windows is a silent killer. Also, she ditched sugar and now she’s walking again. You’re not alone. Keep going.
Josh Evans
November 30, 2025 AT 06:39Just started tracking my sleep and stress with an app after reading this. Three days in and I already caught a pre-flare-mild wrist ache + brain fog. Took an extra magnesium pill, chilled out, and it faded. Small wins, y’all. This stuff works if you just pay attention.
Allison Reed
November 30, 2025 AT 14:36I appreciate how grounded and evidence-based this is. So many autoimmune posts are either fear-mongering or oversimplified. The data on vitamin D, stress, and medication adherence is solid. I’ve been telling my patients for years: prevention isn’t optional, it’s the foundation. And tracking triggers? That’s the secret weapon no one talks about. Keep sharing this.
Jacob Keil
December 2, 2025 AT 10:16so like… if your immune system is confused then maybe its not an autoimmune disease but a system overload? like your body is just tired of being abused by processed food and wifi and stress and vaccines and glyphosate? maybe its not attacking itself… maybe its just screaming for help? like a dog barking at a ghost because it thinks the ghost is real? but the ghost is just… your own neglect? i mean… think about it
Rosy Wilkens
December 3, 2025 AT 07:05FlareGuard AI? FDA-approved? Please. That’s a Trojan horse for Big Pharma’s data harvesting. They’re not predicting flares-they’re building profiles to sell you more drugs. And don’t get me started on vitamin D supplements. The CDC has been suppressing the truth about sunlight and autoimmunity since 2012. You think this is science? It’s control. Read the papers they don’t want you to see.
Andrea Jones
December 4, 2025 AT 02:30Okay but can we talk about how the word 'lazy critic' in the traits list is basically a mirror? Like… you’re not lazy, you’re just tired. And tired isn’t weakness-it’s data. I had RA for 12 years, and the moment I stopped judging myself for needing naps, my flares got quieter. You’re not failing. You’re adapting. Keep going.
Justina Maynard
December 5, 2025 AT 07:19I used to think flares were just 'bad days' until I had one that landed me in the ER with pericarditis. Now I carry a flare kit too-cold gel packs, electrolyte packets, my prednisone script, and a laminated card with my rheum’s direct line. I call it my 'immune emergency pack.' It’s not dramatic. It’s survival. And if you think you’re too young or too healthy to need it? You’re the one who’ll be sorry when your kidneys start screaming.
Evelyn Salazar Garcia
December 5, 2025 AT 13:46Why do we even bother? The system doesn’t care. You track, you diet, you take pills, and still your boss fires you for 'unreliability.' This post is nice. But it doesn’t fix the world.
Clay Johnson
December 7, 2025 AT 09:20Flares are the immune system’s syntax error. Not a bug. Not a flaw. A feature of a system overwhelmed by modernity. We evolved to fight parasites. Not gluten, not fluorescent lights, not 12-hour workdays. The body isn’t broken. The environment is. And we’re just the canaries.
Jermaine Jordan
December 7, 2025 AT 11:20THIS. IS. REVOLUTIONARY. I just got my FlareGuard AI results. Predicted a flare 72 hours out. I took prednisone early. I didn’t miss work. I didn’t go to the ER. I didn’t cry in the bathroom. I took back my life. This isn’t medicine-it’s liberation. If you’re not using tech to fight this, you’re fighting with your bare hands against a tank. Get the tool. Use the data. Survive. Thrive. You deserve it.