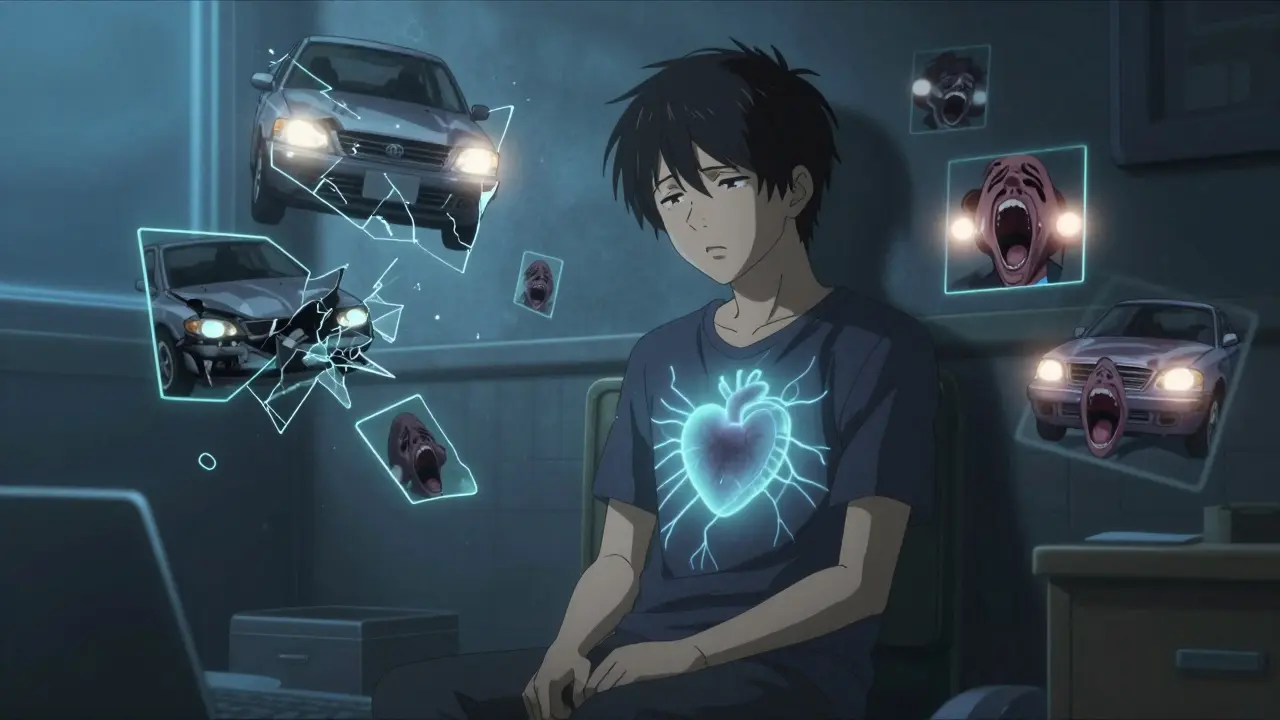
When someone survives a car crash, combat, assault, or any life-threatening event, their brain doesn’t always reset. For about 1 in 10 people, the fear doesn’t fade. It lingers in flashbacks, nightmares, and a constant sense of danger-even when they’re safe. This is post-traumatic stress disorder, or PTSD. It’s not weakness. It’s a biological response to overwhelming trauma. And treating it isn’t about popping a pill and hoping for the best. It’s about understanding how the brain stores trauma, and how medication and therapy can help untangle it.
What PTSD Really Feels Like
PTSD isn’t just feeling sad or anxious after something bad happens. It’s four things happening at once: intrusive memories, avoidance, negative thoughts, and being on high alert all the time. You might relive the event in vivid flashbacks. You might avoid places, people, or even conversations that remind you of it. You might feel numb, guilty, or like the world is unsafe-even if nothing bad has happened in years. And you might jump at every loud noise, sleep poorly, or feel irritable for no reason. The DSM-5-TR, the official guide doctors use to diagnose PTSD, says these symptoms must last more than a month and mess up your job, relationships, or daily life. That’s the threshold. Not everyone who experiences trauma gets PTSD. But for those who do, it’s not something they can just “get over.”Why Therapy Is the First Step
Most experts agree: trauma-focused therapy should come before medication. Why? Because medication can ease symptoms, but it doesn’t process the trauma. Therapy does. Cognitive Processing Therapy (CPT) and Prolonged Exposure (PE) are the two most proven methods. In CPT, you work with a therapist to challenge the thoughts that got stuck after the trauma-like “It was my fault” or “The world is completely dangerous.” You don’t erase the memory. You change how it controls you. Prolonged Exposure is more direct. You slowly, safely, revisit the trauma in your mind, over and over, in sessions. At first, it’s terrifying. But over time, the fear loses its power. The memory becomes just a memory-not a live threat. Studies show 60-70% of people who finish these therapies reach full remission. That’s better than any drug. And the effects last. After therapy ends, symptoms don’t usually come back-unless new trauma hits.What Medications Actually Do
Only two drugs are FDA-approved specifically for PTSD: sertraline (Zoloft) and paroxetine (Paxil). Both are SSRIs-selective serotonin reuptake inhibitors. They don’t cure PTSD. They help you feel calm enough to do the hard work of therapy. Sertraline works for about 53% of people. Paroxetine helps 60%. That means nearly half don’t respond. And even when they do, only 20-30% get completely symptom-free. The rest still struggle with sleep, irritability, or emotional numbness. Other medications are used off-label because they help some people. Venlafaxine (Effexor XR), an SNRI, works just as well as SSRIs in many studies. Mirtazapine and amitriptyline show modest benefits, especially for sleep and nightmares. But they come with side effects: weight gain, drowsiness, dry mouth. Then there’s prazosin. It’s not an antidepressant. It’s a blood pressure drug. But for veterans and others with trauma-related nightmares, it’s a game-changer. In VA studies, half the users cut their nightmare frequency in half within four weeks. No other medication does that. Antipsychotics like risperidone and quetiapine? They’re sometimes added for severe hyperarousal-when you’re constantly tense, angry, or paranoid. But the evidence is shaky. They help a little, but the risks (weight gain, tremors, diabetes) are real.
Medication vs. Therapy: The Numbers Don’t Lie
Let’s compare them side by side.| Factor | Trauma-Focused Therapy | SSRIs (Sertraline/Paroxetine) |
|---|---|---|
| Time to see results | 8-12 weeks | 4-6 weeks |
| Response rate | 60-70% | 50-60% |
| Remission rate | 60-70% | 20-30% |
| Side effects | Mild discomfort during exposure | Nausea, insomnia, sexual dysfunction, emotional blunting |
| Long-term benefit | Yes-effects last after treatment ends | No-relapse is common after stopping |
| Cost (per month) | $100-$200 per session | $4-$10 (generic) |
Therapy costs more upfront. But it’s a one-time investment. Medication is cheaper per month-but you might need it for years. And even then, you’re not healing. You’re managing.
The Real Problem: Side Effects and Dropout
Here’s what no one tells you: nearly one in three people quit SSRIs because of side effects. Sexual dysfunction hits hard-35% lose libido. 28% can’t reach orgasm. Emotional blunting is another silent killer. Some patients say they feel like a zombie-no joy, no sadness, just flat. They stop taking the pill because they don’t feel like themselves. On Reddit’s r/ptsd community, 42% of users who tried SSRIs stopped because of these issues. That’s not failure. That’s a system mismatch. These drugs aren’t designed for trauma. They’re designed for depression. And trauma isn’t depression. That’s why prazosin is so important. It doesn’t touch mood. It doesn’t dull emotions. It just quiets the nightmares. For someone who can’t sleep because they’re reliving an assault or a firefight, that’s not a bonus. It’s survival.When Medication Makes Sense
Therapy isn’t for everyone. Some people are too overwhelmed to start. Others live in constant danger-domestic violence, active combat, unstable housing. In those cases, medication can be a bridge. If you’re too anxious to leave your house, SSRIs might help you get to therapy. If nightmares are destroying your sleep, prazosin might give you enough rest to even think about healing. The VA and DoD guidelines say: try therapy first. But if it’s not possible, or if symptoms are too severe, start medication. And if therapy doesn’t work after 8-12 sessions, add medication. Combining both? That’s where the biggest gains happen. A 2021 JAMA Psychiatry study found 72% of people improved when they got sertraline and prolonged exposure together-better than either alone.
What’s Coming Next
The future of PTSD treatment is already here. MDMA-assisted psychotherapy, once considered experimental, just got FDA Breakthrough Therapy designation. In phase III trials, 67% of participants no longer met PTSD criteria after three sessions with MDMA and therapy. That’s not a miracle. It’s science. Brexpiprazole, an antipsychotic, is being reviewed by the FDA to add to SSRIs for stubborn cases. Early results show a 35% symptom drop when added to existing meds. And then there’s genetics. Researchers have found 95 genetic markers linked to how people respond to SSRIs. In five years, we might test your DNA before prescribing a drug-so you don’t waste months on something that won’t work.What You Can Do Right Now
If you think you have PTSD:- Start with therapy. Look for a provider trained in CPT or PE. The VA offers it for free to veterans. Many nonprofits offer sliding-scale rates.
- If therapy feels impossible, talk to your doctor about prazosin for nightmares or an SSRI for overall anxiety.
- Don’t give up if the first drug doesn’t work. Try another. Sertraline, paroxetine, venlafaxine-each affects people differently.
- Track your symptoms. Use a journal or the VA’s PTSD Coach app. Small improvements matter.
- Be honest about side effects. Sexual dysfunction? Nausea? Emotional numbness? Tell your doctor. There are alternatives.
PTSD isn’t a life sentence. It’s a wound that needs the right kind of care. Medication can quiet the noise. But only therapy can help you hear yourself again.
FAQ
Can PTSD be cured without medication?
Yes. Many people recover fully with trauma-focused therapy alone-especially CPT and Prolonged Exposure. About 60-70% of people who complete these therapies reach remission. Medication isn’t required, but it can help if symptoms are too severe to start therapy.
Why do SSRIs help PTSD if they’re for depression?
PTSD and depression often overlap. Both involve low serotonin, which affects mood, sleep, and anxiety. SSRIs don’t erase trauma, but they reduce the brain’s overreaction to stress. This gives people enough calm to engage in therapy. They’re not a cure, but a tool to make healing possible.
How long should I take PTSD medication?
Most experts recommend staying on medication for at least 12 months after symptoms improve. Stopping too soon leads to relapse in over half of cases. Some people need it longer, especially if they’re still in dangerous situations or haven’t done therapy. Never stop abruptly-work with your doctor to taper slowly.
Is prazosin safe for long-term use?
Yes. Prazosin has been used safely for decades to treat high blood pressure. For PTSD nightmares, low nightly doses (1-15 mg) are well tolerated. Side effects are mild-dizziness, lightheadedness, especially when standing up. These usually fade after a few days. It doesn’t cause addiction or emotional blunting, making it one of the safest options for trauma-related sleep issues.
What if I’ve tried every medication and nothing worked?
You’re not alone. About 1 in 5 people with PTSD don’t respond to standard meds. That’s called treatment-resistant PTSD. The next step is trauma-focused therapy-especially if you haven’t tried it yet. If therapy didn’t work, newer options like MDMA-assisted therapy (available in clinical trials) or ketamine are being studied. Ask your doctor about research programs or specialized PTSD clinics.
Can I use alcohol or marijuana to self-treat PTSD?
No. Alcohol and marijuana might seem to help at first-numbing the pain, helping you sleep. But over time, they make PTSD worse. They interfere with memory processing, increase anxiety, and block the brain’s ability to heal. They also raise the risk of addiction, which doubles the chance of suicidal thoughts. If you’re using substances to cope, talk to your provider. There are safer, proven ways forward.

 Medications
Medications
Janette Martens
December 28, 2025 AT 13:16Marie-Pierre Gonzalez
December 28, 2025 AT 22:13Louis Paré
December 29, 2025 AT 23:37Vu L
December 30, 2025 AT 23:01James Hilton
January 1, 2026 AT 17:08Mimi Bos
January 3, 2026 AT 02:44Payton Daily
January 3, 2026 AT 20:19Kelsey Youmans
January 4, 2026 AT 18:23Sydney Lee
January 5, 2026 AT 22:28oluwarotimi w alaka
January 6, 2026 AT 16:58Debra Cagwin
January 7, 2026 AT 16:01