Flare Triggers: What Causes Medication Flares and How to Manage Them
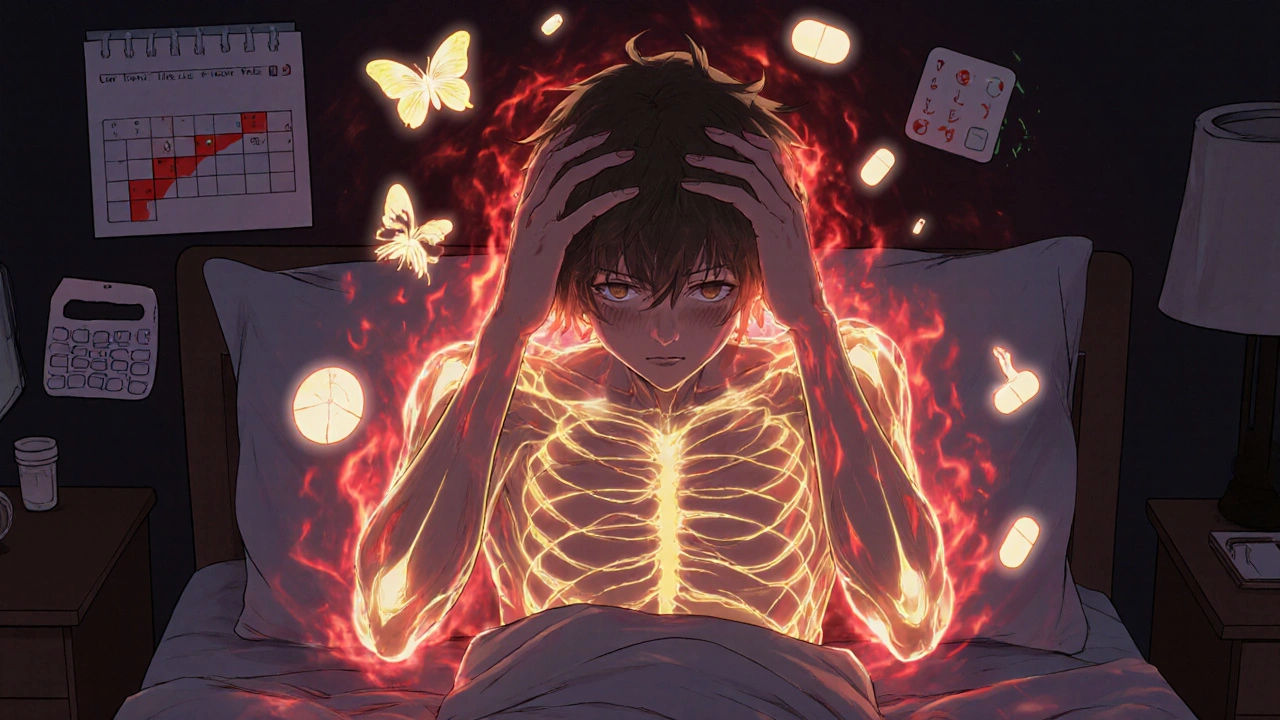
When your body reacts badly to a drug you’ve taken for months—or even years—it’s not just bad luck. It’s a flare trigger, a specific factor that causes a sudden worsening of symptoms due to medication or interaction. These aren’t random events. They’re predictable, often preventable, and tied to things like drug changes, infections, stress, or even what you ate for breakfast. A flare isn’t just discomfort—it can mean hospital visits, missed work, or worse. Think of it like a fuse: the medication might be fine on its own, but add another drug, a cold, or a sleepless night, and boom—your system overloads.
Some flare triggers, specific substances or conditions that provoke sudden adverse reactions in patients are obvious. Clindamycin, for example, is known to trigger C. difficile, a dangerous bacterial infection that causes severe diarrhea and colitis, often after antibiotic use. SGLT2 inhibitors, used for diabetes, can cause euDKA—even when blood sugar looks normal. And switching generics? That’s another hidden flare trigger. Not all generics are created equal. With narrow therapeutic index drugs, even tiny differences in absorption can push your body over the edge. One study found patients on certain generic versions of warfarin had more bleeding events than those on the brand, not because the drug was unsafe—but because the body reacted to the change.
It’s not just drugs. Stress, poor sleep, alcohol, and even seasonal allergies can act as flare triggers. If you’re on beta-blockers and suddenly start taking a first-generation antihistamine like Benadryl, you’re stacking up anticholinergic effects. That combo can spike your heart rate, blur your vision, or make you dizzy. Pregnant women on certain meds? Pregnancy registries track how those drugs interact with hormonal shifts—because a flare during pregnancy can mean risk to the baby. And if you’re managing chronic pain, diabetes, or autoimmune disease, your flare triggers are likely unique to your mix of meds, lifestyle, and biology.
What’s missing from most doctor visits is the connection between your daily habits and your medication response. You might not realize that skipping dinner, drinking grapefruit juice, or taking a new supplement is what’s causing your sudden headache, rash, or spike in blood pressure. Flare triggers don’t care if you’re following the prescription—they care if your body’s balance is off.
This collection of posts dives into the real-world causes of medication flares. You’ll find clear breakdowns of how antibiotics like clindamycin can turn deadly, why switching generics isn’t always safe, and how digital tools help track patterns before a flare hits. We cover the hidden risks of SGLT2 inhibitors, the dangers of mixing antihistamines with heart meds, and how storage mistakes can make controlled substances unsafe. You’ll also learn how to spot early warning signs and what to ask your pharmacist before you take that next pill. No fluff. No theory. Just what actually causes flares—and how to stop them before they start.
Autoimmune flares are unpredictable surges of immune activity that worsen symptoms and disrupt daily life. Learn the top triggers, proven prevention strategies, and early intervention tactics to reduce flare frequency and severity.

 Medications
Medications