Automated Dispensing Cabinets: How Hospitals Use Them to Cut Errors and Save Time
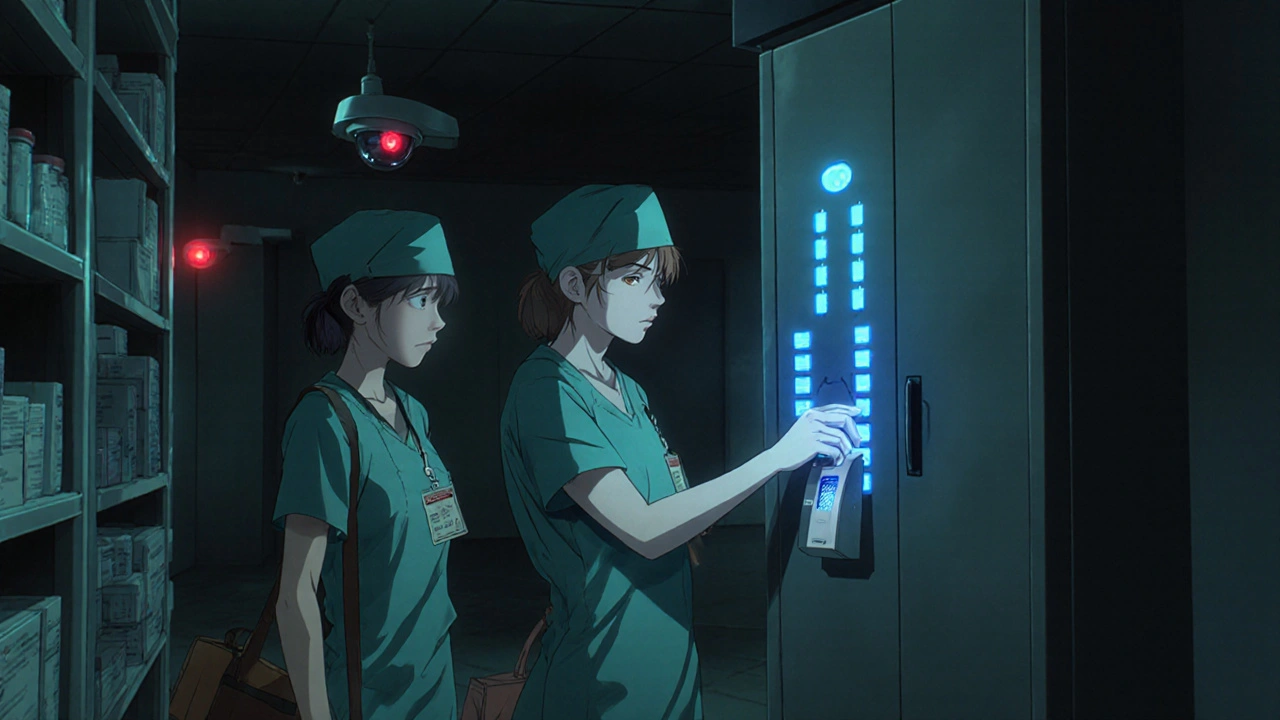
When you think about how hospitals keep meds safe and accurate, you might picture a pharmacist counting pills by hand. But in most modern hospitals, that job is handled by automated dispensing cabinets, computer-controlled systems that store, track, and release medications at the point of care. Also known as ADCs, these locked units sit right on nursing units and give staff instant access to the right drug, in the right dose, at the right time—without leaving the patient’s room. They’re not just fancy pill boxes. They’re a critical layer in the chain of medication safety, reducing mistakes that come from manual counting, mislabeling, or wrong pick-ups.
These cabinets connect to the hospital’s electronic health record and pharmacy system. When a nurse needs a dose, they scan their badge, enter the patient ID, and the cabinet unlocks just the drawer with the correct medication. Some even have built-in barcode scanners that double-check the drug against the patient’s order. If something doesn’t match, the system blocks the release. That’s not theory—it’s real. A 2020 study in Journal of Patient Safety showed hospitals using ADCs cut medication errors by nearly 30% compared to those still using floor stock. And it’s not just about safety. Nurses spend less time walking to the pharmacy and more time with patients. Pharmacists get real-time data on usage patterns, helping them catch trends like overuse of certain antibiotics or sudden spikes in pain med requests.
But ADCs don’t work in a vacuum. They rely on pharmacy automation, the broader use of technology to manage drug inventory, dispensing, and tracking to stay stocked and updated. They also depend on medication safety, the system of protocols, training, and tech designed to prevent harmful errors to function properly. If a nurse skips a scan or a pharmacist doesn’t update the system after a recall, the whole system breaks down. That’s why the posts below cover everything from how to train staff on ADC use, to how drug interactions show up in the data, to why some hospitals still struggle with adoption despite the clear benefits.
You’ll find real examples here: how ADCs helped cut Clindamycin misuse and reduce C. diff outbreaks, how pill organizers and blister packs tie into the same goal of preventing mistakes, and how tools like OpenFDA and FAERS help track what goes wrong when automation fails. Whether you’re a nurse, pharmacist, hospital admin, or just someone curious about how meds get from the pharmacy to your bedside, this collection gives you the practical, no-fluff details on how automated dispensing cabinets are changing care—one locked drawer at a time.
Learn how to securely store controlled substances to prevent theft and diversion in healthcare settings. Follow DEA-compliant practices, use dual control, implement audits, and avoid common pitfalls that put patients and staff at risk.

 Medications
Medications