Drug Interaction Checker
Check Your Medication Safety
Enter medications you're currently taking to identify potential interactions and dangerous combinations.
Results
Why Your Medication Might Be Causing Worse Side Effects Than Expected
You take your blood pressure pill every morning. You’ve been on it for years. But lately, you’ve been feeling dizzy, tired, and your muscles ache more than usual. You didn’t change your dose. You didn’t start a new supplement. So why now? The answer might be hiding in your medicine cabinet.
Drug interactions are one of the most common - and preventable - reasons side effects get worse. It’s not always about the drug itself. It’s about what else you’re taking with it. A simple combination of two perfectly safe medications can turn mild side effects into something dangerous. And most people don’t even know it’s happening.
How Drug Interactions Actually Work
When two or more drugs are taken together, they can interfere with how your body handles each one. This isn’t magic. It’s biology. Your liver uses enzymes - especially a group called cytochrome P450 - to break down medications so they can leave your system. One drug might slow down that process, causing another to build up to toxic levels.
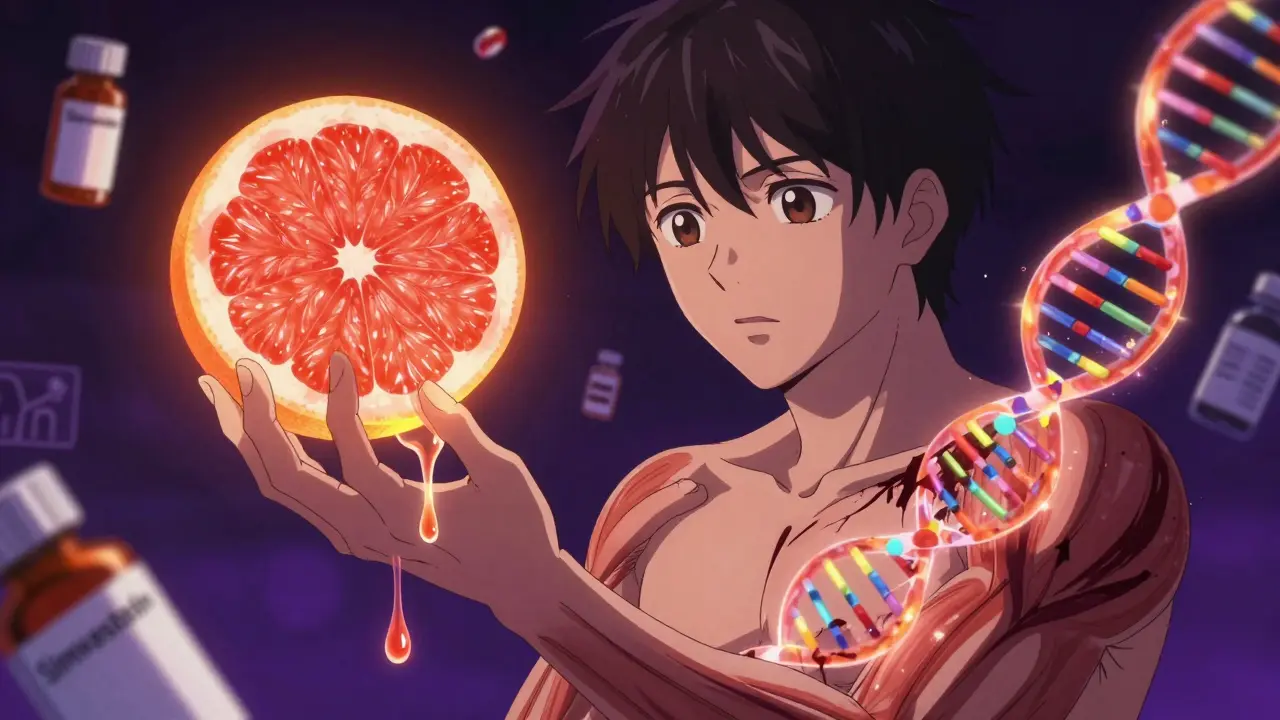
The biggest player here is CYP3A4. It’s responsible for breaking down about half of all prescription drugs, including statins, blood thinners, and many antidepressants. If you take something that blocks CYP3A4 - like grapefruit juice, clarithromycin, or even some antifungal pills - your body can’t clear the other drug fast enough. That’s when side effects spike.
Take simvastatin, a common cholesterol drug. When taken with clarithromycin (an antibiotic), the risk of severe muscle damage (rhabdomyolysis) jumps by more than eight times. That’s not a small risk. It’s life-threatening. Azithromycin, another antibiotic, doesn’t do this. So why take the dangerous one? Because many doctors don’t realize the difference.
Common Dangerous Combinations You Might Not Know About
- Warfarin + aspirin or NSAIDs: Warfarin thins your blood. Aspirin and ibuprofen also thin it. Together, they can cause internal bleeding. Studies show this combo increases bleeding risk by 70-100%.
- SSRIs + tramadol or dextromethorphan: These are found in many pain relievers and cough syrups. Mixing them can trigger serotonin syndrome - a dangerous spike in brain chemicals that causes confusion, rapid heartbeat, seizures, and even death.
- Statin + grapefruit juice: One grapefruit can raise statin levels by up to 300%. Muscle pain? That’s not just a side effect - it’s a warning sign your body is drowning in the drug.
- Warfarin + vitamin K supplements: Vitamin K reverses warfarin’s effect. If you start eating more kale, spinach, or take a supplement without telling your doctor, your INR can crash. You’re no longer protected from clots.
- Alprazolam + alcohol: Both depress the central nervous system. Together, they can slow your breathing to dangerous levels. This isn’t just risky - it’s deadly.
Genetics Play a Bigger Role Than You Think
Not everyone reacts the same way to drug combinations. Why? Because your genes control how fast or slow you metabolize medications. About 3-10% of white people are “poor metabolizers” of CYP2D6 - an enzyme that processes codeine, antidepressants, and some heart drugs.
If you’re one of them and you take codeine, your body can’t convert it to morphine properly. Instead, it builds up as the original drug, causing nausea, dizziness, and even respiratory depression. On the flip side, some people are “ultra-rapid metabolizers.” They turn codeine into morphine too fast - leading to overdose even at normal doses.
The FDA now requires pharmacogenetic warnings on 30% of commonly prescribed drugs. That means your doctor should be checking your genetic profile if you’re on multiple meds. But most still don’t. It’s not because they’re careless. It’s because the tools aren’t widely used.
Food, Supplements, and Even Herbal Teas Can Trigger Reactions
It’s not just pills. Grapefruit juice is the most famous offender, but it’s not alone. St. John’s wort - a popular herbal remedy for depression - can make birth control, HIV meds, and transplant drugs useless. It forces your body to break them down too fast.
Calcium-rich foods like milk or yogurt can block antibiotics like tetracycline and ciprofloxacin from being absorbed. If you take them with breakfast, you might as well not take them at all. The absorption drops by 50-90%.
Even green tea and cranberry juice can interfere with blood thinners. And don’t assume “natural” means safe. Many herbal supplements are unregulated, and their effects on drug metabolism are poorly studied.
Why Doctors Miss These Interactions
Here’s the uncomfortable truth: your doctor probably doesn’t know about all the drugs you’re taking. Patients forget to mention over-the-counter meds, supplements, or even occasional alcohol use. One study found that 68% of hospitalized patients had at least one dangerous drug interaction - and nurses caught 40% of them that doctors missed.
Electronic health records are supposed to help. They flag interactions. But they flag too much. A 2019 JAMA study found that 40% of alerts are for low-risk combinations that don’t matter. Doctors start ignoring them. It’s called alert fatigue. By the time a real danger pops up, the system is already drowned in noise.
And even when alerts are right, doctors don’t always act. Why? Because changing a prescription feels risky. They worry about upsetting the patient, or think, “It’s never caused a problem before.” But that’s how disasters happen.
What You Can Do Right Now
- Make a full list of everything you take: Prescription, over-the-counter, vitamins, herbs, even occasional alcohol or CBD. Write it down. Don’t rely on memory.
- Bring it to every appointment: Ask, “Could any of these interact?” Don’t wait for the doctor to ask. They’re busy. You’re the one living with the side effects.
- Use a free interaction checker: Sites like Medscape or Drugs.com have tools you can use at home. Type in your meds. See what pops up. If something looks risky, ask your pharmacist.
- Ask about alternatives: If you’re on a drug with 50+ known interactions, ask if there’s a safer option. For example, azithromycin instead of clarithromycin. Or pravastatin instead of simvastatin.
- Get tested if you’re on long-term meds: Especially if you’re over 65, taking five or more drugs, or have unexplained side effects. Pharmacogenetic testing is becoming more affordable and accessible.
How the System Is Changing - And How You Can Benefit
Big changes are coming. AI models are now predicting dangerous drug combos with 89% accuracy - far better than old databases. The NIH is rolling out pharmacogenetic prescribing in 15 health systems. Early results show a 36% drop in high-risk interactions.
Wearable sensors that monitor drug levels in real time are in trials. Imagine a patch that tells your doctor your warfarin level is spiking - before you bleed. That’s not science fiction. It’s next year’s reality.
But none of this matters if you don’t speak up. The system is improving, but it still relies on you to be your own advocate. You’re the only one who knows how you feel. You’re the only one who can notice the new fatigue, the strange bruising, the muscle pain that won’t go away.
Bottom Line: Side Effects Aren’t Always About the Drug
Medications are powerful tools. But they’re not harmless. And their risks multiply when mixed. The good news? Most dangerous interactions are preventable. You don’t need to be a doctor to protect yourself. You just need to be informed - and willing to ask questions.
If you’re taking more than three medications, you’re at higher risk. If you’re over 65, you’re at even higher risk. Don’t wait for a crisis. Start today. Make your list. Talk to your pharmacist. Ask about alternatives. Your body will thank you.
Can drug interactions happen even if I take my meds at different times of day?
Yes. Some interactions aren’t about timing - they’re about your body’s chemistry. For example, grapefruit juice blocks the CYP3A4 enzyme for up to 72 hours. So even if you take your statin at night and drink grapefruit juice in the morning, the interaction still happens. The same goes for drugs that build up over time, like warfarin or antidepressants. It’s not when you take them - it’s how your body processes them together.
Are over-the-counter drugs safer than prescriptions when it comes to interactions?
No. Many OTC drugs are just as risky. Ibuprofen, naproxen, and aspirin can all increase bleeding risk with blood thinners. Antihistamines like diphenhydramine can worsen drowsiness when mixed with opioids or benzodiazepines. Even common supplements like St. John’s wort or vitamin K can interfere with prescription drugs. Just because it’s sold without a prescription doesn’t mean it’s harmless.
Why do some people have side effects from a drug combination while others don’t?
It comes down to genetics, age, liver and kidney function, and what else you’re eating or drinking. Two people taking the same two drugs can have completely different outcomes. One might feel fine. The other ends up in the hospital. That’s why blanket warnings don’t always work. Personalized care - knowing your unique biology - is the only way to predict risk accurately.
How do I know if a side effect is from a drug interaction and not just the medication itself?
Look at timing. Did the side effect start or get worse after you added a new pill, supplement, or changed your diet? If you’ve been on a drug for months with no issues, but suddenly feel worse after starting a new antibiotic or switching to a different pain reliever, that’s a red flag. Talk to your pharmacist - they’re trained to spot these patterns.
Is it safe to stop a medication if I suspect an interaction?
Never stop a prescription drug without talking to your doctor. Some drugs, like blood pressure or seizure meds, can cause serious withdrawal effects. But you can - and should - ask your doctor to review your list. Say: “I think something I started recently might be making my side effects worse.” That’s a safe way to start the conversation without risking your health.

 Medications
Medications
Lisa McCluskey
January 31, 2026 AT 11:35owori patrick
January 31, 2026 AT 15:25