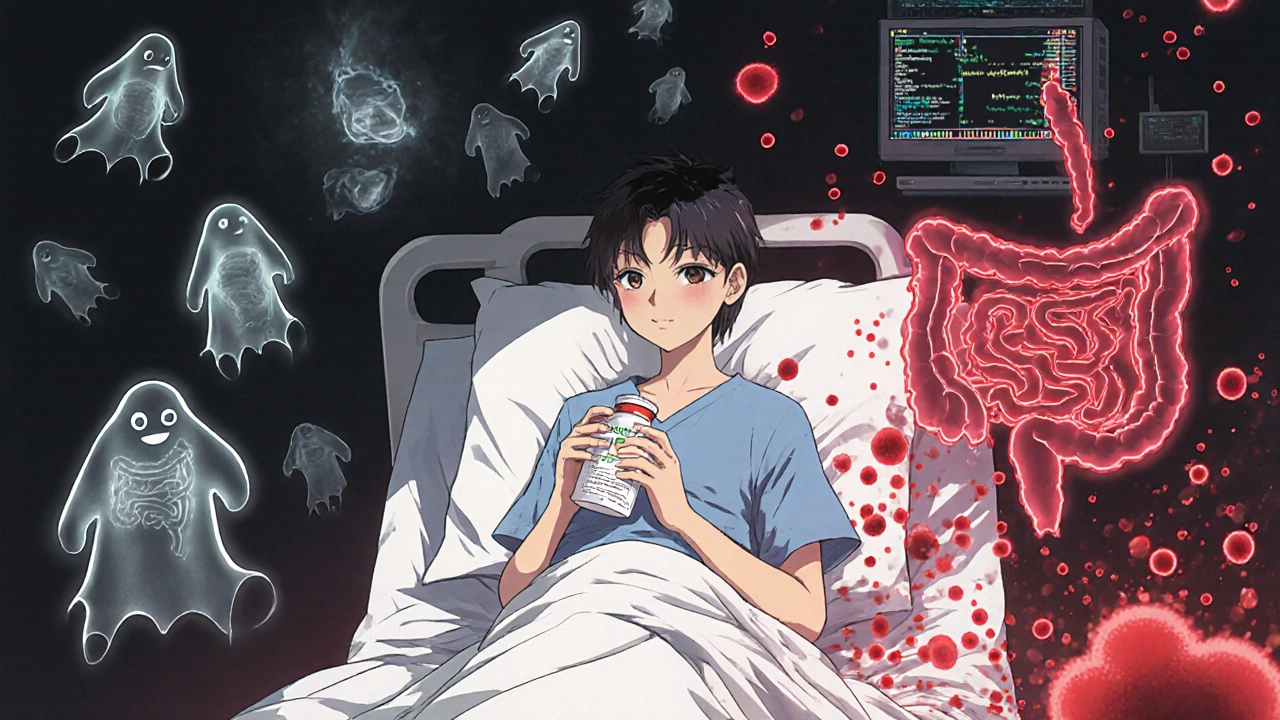
Antibiotic Diarrhea: What It Is, Why It Happens, and How to Handle It
When you take an antibiotic diarrhea, a digestive side effect caused by antibiotics disrupting the natural balance of gut bacteria. Also known as antibiotic-associated diarrhea, it’s not just an inconvenience—it’s a sign your gut microbiome is under stress. About 20% of people who take antibiotics end up with loose stools, and while it often goes away on its own, sometimes it’s a warning sign of something more serious.
This isn’t just about irritation. Antibiotics don’t pick and choose—they wipe out both bad and good bacteria. That’s where Clostridium difficile, a dangerous bacterium that can overgrow when normal gut flora is wiped out. Also known as C. diff, it causes severe diarrhea, fever, and even life-threatening colon damage. It’s not rare. Hospitals see hundreds of cases every year, especially in older adults or those on long-term antibiotics. Even a short course of amoxicillin or ciprofloxacin can trigger it. And here’s the catch: not all diarrhea from antibiotics is the same. Mild cases might just mean a few loose stools. Severe cases involve watery diarrhea multiple times a day, abdominal cramps, and sometimes blood.
That’s why knowing the difference matters. If you start having diarrhea while on antibiotics—or even a few days after finishing—you can’t just wait it out. You need to know when to call your doctor. And you need to know what actually helps. probiotics, live microorganisms that help restore gut balance after antibiotic use. Also known as good bacteria supplements, they’re not magic, but studies show certain strains like Lactobacillus rhamnosus and Saccharomyces boulardii can reduce the risk of antibiotic diarrhea by up to 60%. Not all probiotics are equal, and not all yogurt will do the trick. The right strain, at the right dose, taken at the right time, makes a real difference.
What you eat also plays a role. Sugary foods and processed carbs feed the bad bugs. Fiber-rich foods like oats, bananas, and cooked vegetables support recovery. Hydration isn’t optional—it’s critical. Dehydration from diarrhea can hit fast, especially in older adults. And skipping your next antibiotic dose because of diarrhea? That’s dangerous. Never stop antibiotics without talking to your doctor, even if you feel worse. Stopping early can make the infection come back stronger.
The posts below cover exactly this: how antibiotics mess with your gut, what to watch for, which probiotics actually work, how to prevent C. diff, and what alternatives exist when antibiotics aren’t the only option. You’ll find real-world advice from people who’ve been there, and clear explanations of what science says—not hype, not guesses. Whether you’re taking antibiotics now, had diarrhea after a course, or just want to protect your gut before your next prescription, this collection gives you the facts you need to act wisely.
Clindamycin carries the highest risk of triggering C. difficile infection among antibiotics. Learn the warning signs, when to seek emergency care, and how to protect yourself after taking this common drug.

 Medications
Medications