When a pharmacist swaps a brand-name drug for a generic, most patients don’t think twice. But for NTI drugs, that simple switch can carry serious risks. Narrow Therapeutic Index (NTI) drugs are medications where even tiny changes in dosage or blood levels can cause treatment to fail-or trigger dangerous side effects. Think warfarin, lithium, phenytoin, levothyroxine, and tacrolimus. These aren’t just any pills. They’re the kind where 10% more or less in your bloodstream could mean the difference between stability and hospitalization.
Why NTI Drugs Are Different
Not all generics are created equal. The FDA defines NTI drugs as those where the gap between the minimum effective dose and the minimum toxic dose is two or less. That’s razor-thin. For most medications, generics are approved if they’re within 80-125% of the brand’s absorption rate. But for NTI drugs? The bar is higher. Since 2019, the FDA requires generics to stay within 90-111%-a tighter range designed to reduce variability.
Still, many prescribers don’t trust that margin. A 2021 survey of internists found that 57% would choose the brand-name version when starting a high-risk patient on an NTI drug. Why? Stability. Once a patient’s levels are balanced-say, their INR steady on warfarin or their lithium level stable-doctors fear any switch might throw that balance off. Even if the science says it’s safe, the fear of a bad outcome lingers.
Doctors vs. Pharmacists: A Gap in Trust
There’s a disconnect between what pharmacists believe and what doctors feel. A 2018 study showed that 87% of pharmacists thought physicians saw generics as equally effective. But only 60% of pharmacists routinely substituted generics for refills-suggesting they knew doctors were hesitant. Meanwhile, 94% of pharmacists believed doctors considered generics equally safe. Yet, transplant specialists, who deal with drugs like tacrolimus daily, were far less confident. One 1997 survey found 92% of transplant pharmacists believed bioequivalence tests on healthy volunteers didn’t reflect real-world patient responses.
It’s not that doctors are anti-generic. They’re pro-safety. Many rely on therapeutic drug monitoring-regular blood tests-to keep levels in range. But those tests cost time, money, and stress. A 2022 study by MGMA estimated each NTI substitution incident led to an extra $127 in monitoring costs per patient. And 41% of physicians reported patients got confused after a switch, showing up confused or anxious, asking if the new pill was “the same.”
State Laws Are Split-And So Are Prescribers
Twenty-eight U.S. states have rules around NTI substitution. Some, like Texas and Florida, keep official lists of NTI drugs and block automatic swaps unless the prescriber says otherwise. Seventeen states require patient consent before switching. In those states, generic substitution rates for NTI drugs are 23% lower than in states with no restrictions.
The American Medical Association (AMA) says the current system works fine. They argue that with proper monitoring, switching is safe for most patients. But the American Academy of Neurology disagrees. Their 2019 guidelines say automatic substitution for drugs like levothyroxine and phenytoin should require prescriber input. And the American Society of Health-System Pharmacists found that 78% of hospital pharmacists always notify doctors before substituting an NTI drug-because they know how nervous prescribers are.
Real-World Data vs. Regulatory Confidence
The FDA insists generics are safe. In 2020, their Center for Drug Evaluation and Research reported that 98% of NTI generics perform within 3-4% of the brand. That’s tight. And post-market surveillance hasn’t shown widespread harm. The Institute for Safe Medication Practices logged 1,247 NTI-related errors between 2015 and 2020-but only 8% led to actual patient harm.
Still, the numbers don’t erase the fear. When you’re managing a heart transplant patient on tacrolimus, you don’t want to rely on averages. You want certainty. That’s why brand-name tacrolimus still holds a 32% market share despite generic availability. Same with warfarin-28% of prescriptions are still for the brand. These aren’t just cost-driven choices. They’re risk-averse ones.
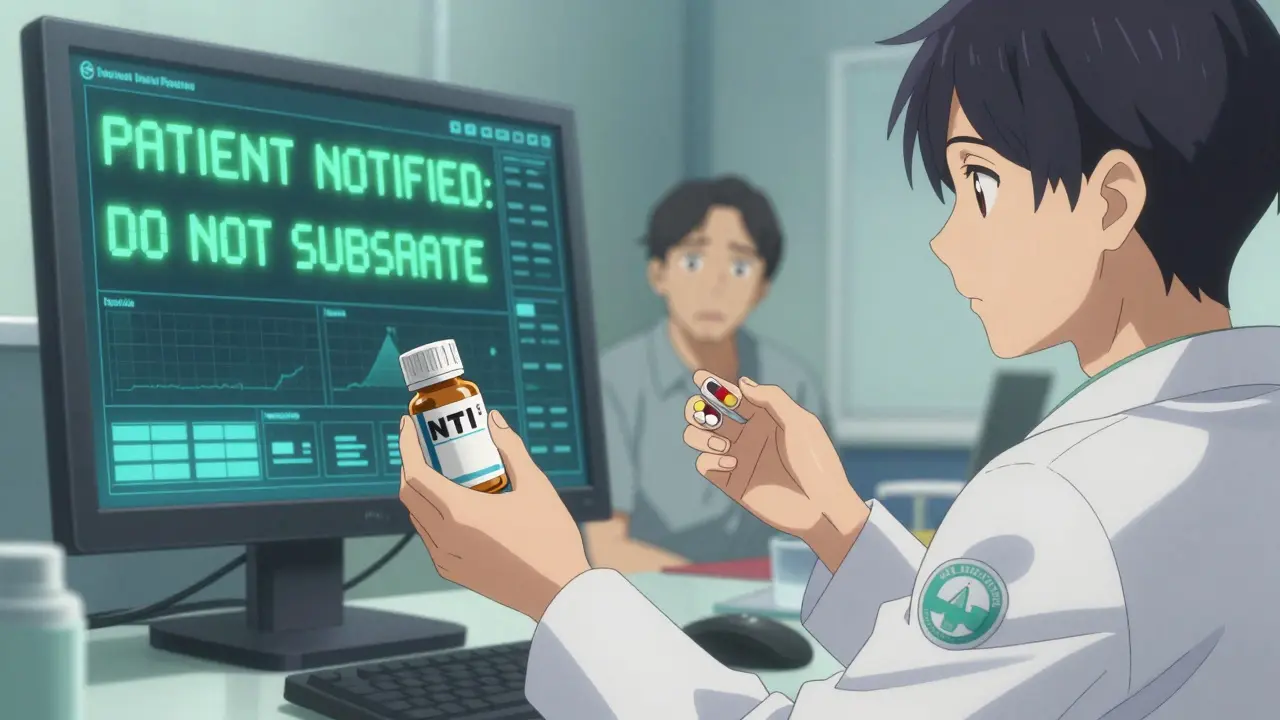
Communication Is the Missing Link
One big issue? Lack of clear communication. Most physicians don’t get notified when a substitution happens. A 2021 study found that 63% of doctors prefer electronic alerts over phone calls. Primary care physicians get about 2.7 NTI substitution notices a month. Psychiatrists managing lithium? That jumps to 5.4. That’s a lot of alerts. And many systems don’t send them at all.
Dr. Michael Cohen of the Institute for Safe Medication Practices pointed out that NTI drugs often lack clear labeling. No universal symbol. No standardized warning. That makes it easy for a pharmacist to miss a critical flag. Prescribers want better tools-electronic flags in EHRs, automatic alerts, clear documentation. Not more rules. Just better systems.

What’s Changing in 2026?
Things are shifting. In March 2023, the FDA added 12 new drugs to its NTI list and removed three based on new data. The Centers for Medicare & Medicaid Services proposed a rule in late 2023 requiring prescriber notification for all NTI substitutions under Medicare Part D. That’s a big move-it means federal policy may soon align with what many doctors have been asking for.
Meanwhile, the PRESCRIPT-NTI trial, enrolling 1,200 patients across 42 sites, is tracking clinical outcomes after substitution. Early results are expected in mid-2024. If the data shows no increase in adverse events, it could ease fears. But if it shows even small spikes in hospitalizations or lab abnormalities, it could trigger stricter rules.
And in oncology? The American Society of Clinical Oncology now supports generic substitution for oral NTI cancer drugs-so long as therapeutic drug monitoring is in place. That’s a sign of changing attitudes. As more real-world evidence accumulates, some specialists are becoming more comfortable.
What This Means for You
If you’re on an NTI drug, don’t assume your pharmacist will ask your doctor before switching. In many states, they don’t have to. If you’re on warfarin, lithium, or tacrolimus, ask your prescriber: “Is this drug on your list of ones I shouldn’t switch?” If they say yes, ask them to write “Dispense as written” or “Do not substitute” on your prescription.
And if you’re a provider? Consider using your EHR to flag NTI drugs. Add a note to your templates. Train your staff. Make substitution a conversation, not a default. Because for these drugs, the difference between “safe” and “risky” isn’t always in the pill-it’s in the communication.
Market Trends and the Bottom Line
Generic use for NTI drugs is climbing. In 2023, 62% of prescriptions were generic. By 2028, industry analysts predict that number will hit 78%. But the remaining 22%? Those are the patients and prescribers who aren’t convinced. And they’re not just clinging to brand names out of habit. They’re reacting to real-world experience, fragmented data, and a system that still doesn’t talk clearly between doctors, pharmacists, and patients.
The economic argument is strong: restricting substitution could cost Medicare $1.2 billion a year. But the safety argument? It’s personal. For the patient whose INR spikes after a switch, it’s not about savings. It’s about survival.
The future of NTI substitution isn’t about banning generics. It’s about building trust-through better labeling, smarter alerts, consistent monitoring, and, above all, clear communication between the people who write the script and the ones who fill it.


 Medications
Medications
LIZETH DE PACHECO
January 3, 2026 AT 01:53I’ve been on warfarin for 8 years. Switched generics twice-both times my INR went nuts. Had to go to the ER. Now my doc writes 'Do not substitute' on every script. No debate. I don’t care if it’s cheaper. My life isn’t a cost-benefit analysis.
Pharmacists mean well, but they’re not the ones lying awake wondering if they’ll bleed out tonight.
Lee M
January 3, 2026 AT 03:27Let’s be real-the FDA doesn’t give a damn about your INR. They care about patent cliffs and corporate profits. The ‘90-111%’ range? That’s not science, that’s a loophole. They test generics on healthy college kids, then slap ‘bioequivalent’ on a bottle meant for someone with a transplanted heart.
This isn’t about trust. It’s about corporate greed masquerading as regulation. Wake up.
Kristen Russell
January 5, 2026 AT 03:10My dad’s on lithium. Switched generics once. He got dizzy, forgot his own birthday. We caught it early, but I’ll never forget the look in his eyes. Now we fight for brand. Not because we’re rich-we’re not. But because safety isn’t negotiable.
Doctors, pharmacists, patients-we all want the same thing. We just need better systems, not more rules.
Matthew Hekmatniaz
January 6, 2026 AT 05:13I work in a VA hospital. We’ve got patients on tacrolimus, phenytoin, you name it. We don’t substitute unless the prescriber signs off-and even then, we call them. It’s not bureaucracy. It’s respect.
These aren’t aspirin. These are precision instruments. You wouldn’t swap a Ferrari engine for a knockoff and say ‘it’s close enough.’ Why do it with someone’s life?
sharad vyas
January 7, 2026 AT 19:18in india we dont have much generic problem. all medicine is cheap. but i see in usa people fight over pill color. i think maybe you need better doctor not better pill.
my uncle take same medicine for 20 year. no problem. he dont care brand or generic. he care his body feel good.
Dusty Weeks
January 9, 2026 AT 07:20they’re lying to us. 😡
the FDA is in bed with big pharma. brand-name makers pay them to keep generics out. that’s why they made the 90-111 rule-just enough to pretend it’s safe. watch. in 2026 they’ll say ‘oh we were wrong’ and blame the pharmacists.
also-why no universal symbol? because they don’t want you to notice. 🤫
ask yourself: who profits if you get sick?
Sally Denham-Vaughan
January 10, 2026 AT 07:52My pharmacist once switched my levothyroxine without telling me. I gained 15 lbs in 3 weeks. Thought I was depressed. Turned out my TSH was through the roof.
Now I ask every time. Even if they roll their eyes. Better to be annoying than dead.
Also-why is it so hard to get an alert in the EHR? It’s 2024. We have self-driving cars. Can’t we have a pop-up that says ‘NTI DRUG-DO NOT SUB’?
gerard najera
January 11, 2026 AT 10:19It’s not the drug. It’s the monitoring. If you’re not testing regularly, no pill is safe.
Stephen Gikuma
January 12, 2026 AT 11:47They want you to believe generics are fine. But why do the same doctors who push them for statins refuse them for tacrolimus? Coincidence? Nah. It’s the deep state. Globalists want you dependent on their meds. Cheap pills? No. Controlled pills. That’s the game.
They’re coming for your thyroid next. Get ready.
Bobby Collins
January 13, 2026 AT 03:49My sister got switched to generic warfarin and ended up in ICU. The pharmacy didn’t even tell her. She thought it was the same pill. They don’t care. They just want to hit their quota.
And now they’re pushing this ‘2026 rule’ like it’s a gift? It’s a trap. They’ll use it to track you. Every substitution logged. Who you are. What you take. Where you live.
They’re building the database. Don’t fall for it.
Layla Anna
January 14, 2026 AT 22:57i just want to say thank you to all the doctors who still write 'do not substitute' even when it's a hassle
and to pharmacists who call you before switching
you're the quiet heroes in this mess
and to patients who speak up-keep doing it
we need more of you ❤️