When you pick up a generic pill from the pharmacy, you might wonder: is this really the same as the brand-name drug you’ve been taking? The answer isn’t just yes - it’s backed by strict science, decades of data, and a regulatory system designed to make sure you get the exact same effect, no matter the price tag.
What Does ‘Same Absorption Rate’ Actually Mean?
It’s not about looking the same. It’s not even about tasting the same. It’s about how your body absorbs the medicine. That’s called bioequivalence. For a generic drug to be approved, it must deliver the same amount of active ingredient into your bloodstream at the same speed as the brand-name version. Not close. Not mostly. Exactly.
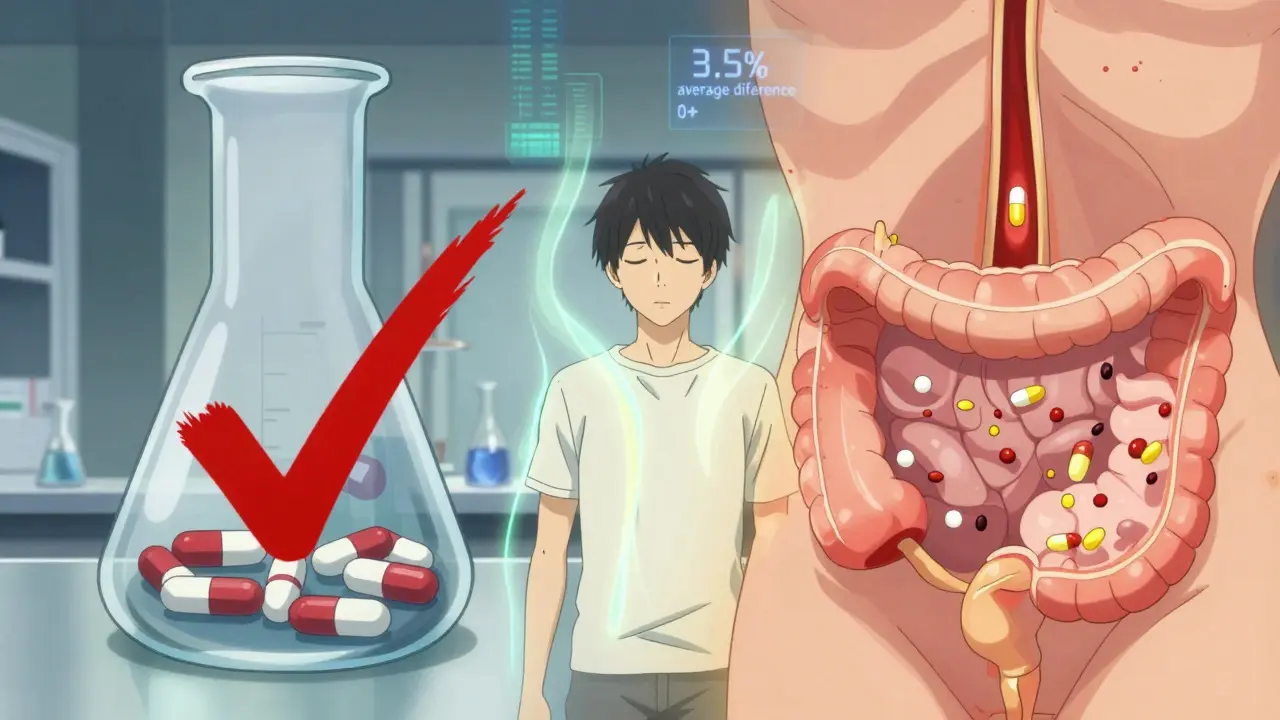
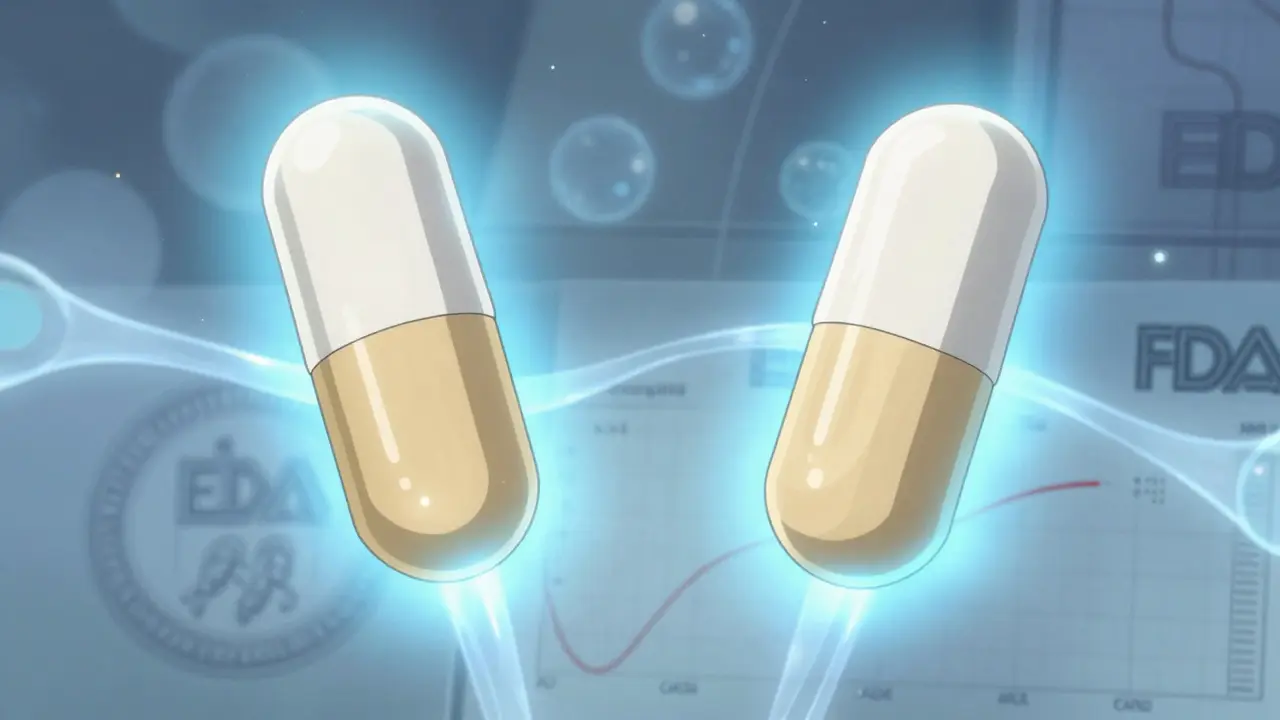
The FDA requires two key measurements: AUC and Cmax. AUC - Area Under the Curve - tells you how much of the drug your body absorbs over time. Cmax - the peak concentration - tells you how fast it gets there. Both must fall within 80% to 125% of the brand-name drug’s values. That’s not a 45% range like some people think. It’s a statistical window that forces the average difference to be tiny.
Here’s what the numbers show: across more than 2,000 studies, the average difference in absorption between generic and brand drugs was just 3.5%. For AUC, it was 3.56%. For Cmax, it was 4.35%. In nearly 98% of cases, the generic differed by less than 10%. That’s less variation than you’d see if you took the same brand-name pill twice on different days.
Why the 80-125% Rule Exists
This range wasn’t picked out of thin air. It’s based on how your body naturally absorbs drugs. Even when you take the exact same brand-name pill twice, your absorption can vary by 10-15% due to things like what you ate, your metabolism, or even your gut bacteria. The FDA built the 80-125% rule around that real-world biological noise. If a generic’s absorption falls outside that range, it’s not just different - it’s statistically unlikely to behave the same in your body.
And here’s the catch: the rule isn’t about individual test results. It’s about the 90% confidence interval. That means if you run a study with 24-36 healthy volunteers, the entire range of likely results for the generic must fit inside that 80-125% window. If even one end of that range spills out, the drug gets rejected. No exceptions. No compromises.
Dissolution Isn’t Absorption - And That’s Where People Get Confused
Some generics dissolve slower or faster in a lab test than the brand-name version. A 2014 study found that over half of tested generics had different dissolution rates. Generic nifedipine dissolved slower. Generic amoxicillin dissolved faster. That sounds alarming - until you realize dissolution isn’t absorption.
Dissolution is what happens in a beaker. Absorption is what happens in your body. A pill might dissolve quickly in water but still take time to get into your blood. Or it might dissolve slowly but absorb just as well once it reaches your gut. That’s why the FDA doesn’t care about dissolution alone. It only cares about what happens in people - the in vivo data. And time and again, even when dissolution profiles differ, the absorption numbers match.
What About Those ‘Bad’ Generics?
You’ve probably heard stories. Someone switched to a generic antidepressant and felt worse. Or a thyroid patient says their energy dropped after switching. These aren’t myths - but they’re rare, and they’re rarely about bioequivalence.
The FDA has approved over 14,000 generic drugs since 2008. Only 12 cases ever raised a red flag for possible therapeutic failure. That’s a 0.08% failure rate. Most of those cases involved narrow therapeutic index (NTI) drugs - medicines where even a tiny change in blood level can cause harm. For drugs like warfarin, digoxin, and phenytoin, the FDA requires a tighter range: 90-111% for AUC. That’s because a 5% drop in blood level could mean a clot. A 5% rise could mean bleeding.
That’s why pharmacists are trained to check the FDA’s Orange Book. Drugs labeled with an ‘A’ rating are considered therapeutically equivalent. ‘B’ ratings mean there’s a documented issue - and those are the ones doctors sometimes avoid switching patients onto. But even ‘B’ ratings are rare. Most generics are ‘A’.
Why Do People Think Generics Don’t Work?
It’s not the science. It’s the perception. A 2024 analysis of 1,247 patient reviews found 12% reported feeling worse on generics. But here’s the twist: 34% of those complaints were about generic levothyroxine. That’s not because the drug is different - it’s because thyroid medication is incredibly sensitive. Even a 10% change in absorption can shift hormone levels enough to cause symptoms. That’s why doctors often stick with one brand or one generic for thyroid patients - not because generics are unreliable, but because consistency matters more than cost.
Also, generics can look different. Color, shape, size - all changed to avoid trademark infringement. If you’ve been taking a blue oval pill for years and suddenly get a white capsule, your brain might think something’s wrong. That’s not the drug. That’s your mind. Studies show placebo effects are strong in medication use. If you believe the generic is inferior, you’re more likely to feel it.
What About Cost and Access?
Generics aren’t just safe - they’re essential. They make up 90% of all prescriptions filled in the U.S. But they cost only 23% of what brand drugs do. The average copay for a generic is under $20. For brand drugs? It’s often over $100. That’s why 90% of patients stick with generics when given the choice. And when they do, they’re far less likely to abandon their treatment.
A 2019 report found new patients were 266% more likely to stop taking a brand-name drug than a generic - not because generics don’t work, but because they can’t afford the brand. Generics keep people on their meds. That’s not just smart economics. It’s public health.
What’s Changing in 2026?
The FDA is moving toward smarter testing. Instead of always using 30 healthy volunteers for every drug, they’re starting to use computer models and simulations. For complex drugs like inhalers or topical creams, new methods are being developed to measure absorption without human trials. This won’t lower standards - it’ll make testing faster and more precise.
And while the 80-125% rule stays the same for small-molecule generics, biosimilars (generic versions of biologic drugs like insulin or rheumatoid arthritis meds) are under closer watch. Their standards are still evolving, but the core principle remains: if it doesn’t work the same in your body, it doesn’t get approved.
What Should You Do?
If you’re on a generic drug and feel fine - keep taking it. If you switch and notice a change - talk to your doctor. Don’t assume it’s the drug. Check if it’s a new manufacturer. Some generics come from different factories, even if they have the same name. Your pharmacist can tell you if the batch changed.
For NTI drugs, ask your doctor if you should stick with one version. Don’t switch back and forth unless you’re monitored. For everything else? Trust the data. The FDA doesn’t approve generics because they’re cheaper. They approve them because they’re proven to be the same.
Generics aren’t second-rate. They’re science-backed, rigorously tested, and clinically identical. The only real difference? The price. And that’s the win for you - and the healthcare system.
Are generic drugs really as effective as brand-name drugs?
Yes. Generic drugs must meet the same strict bioequivalence standards as brand-name drugs. They deliver the same active ingredient at the same rate and extent into your bloodstream. Studies show the average difference in absorption is just 3-4%, far less than the natural variation you’d see taking the same brand-name drug twice.
Why do some people say generics don’t work for them?
Sometimes, it’s not the drug - it’s the mind. Changing pill shape, color, or size can trigger a placebo effect. Other times, it’s switching between different generic manufacturers, which can cause slight variations in fillers or coatings - though still within safe limits. For narrow therapeutic index drugs like levothyroxine or warfarin, even small changes can cause symptoms, so consistency matters. Always report changes to your doctor, but don’t assume the generic is faulty.
What’s the difference between dissolution and absorption?
Dissolution is how fast a pill breaks down in water - a lab test. Absorption is how fast and how much of the drug enters your bloodstream - what actually matters. A generic might dissolve faster or slower than the brand, but if your body absorbs the same amount at the same rate, it’s still bioequivalent. The FDA only cares about absorption, not dissolution.
Are all generics the same?
All approved generics meet the same FDA bioequivalence standards, so they’re equally effective. But different manufacturers may use different inactive ingredients, which can affect how the pill feels or tastes. Some people report side effects from fillers, not the active drug. If you have a reaction, ask your pharmacist if you can switch to a different generic brand.
Can I switch between different generic brands?
For most drugs, yes. But for narrow therapeutic index drugs like warfarin, lithium, or phenytoin, it’s safer to stick with one brand or generic. Switching can cause small changes in blood levels that may lead to side effects or reduced effectiveness. Always check with your doctor before switching, especially if you’re on a sensitive medication.
How does the FDA ensure generics stay safe after approval?
The FDA monitors all drugs through its Adverse Event Reporting System. If reports suggest a generic is causing unexpected problems, they can request new studies, inspect manufacturing sites, or even pull the drug. Since 2008, only 12 out of over 14,000 approved generics have raised safety concerns - a failure rate of 0.08%.

 Medications
Medications
Yanaton Whittaker
January 31, 2026 AT 11:24LOL at people who still think generics are 'fake medicine' 😂 I switched to generic levothyroxine last year and saved $180/month. My TSH is STILL perfect. If your body can't tell the difference between two identical pills, why are you crying? 🇺🇸💪
Kathleen Riley
February 2, 2026 AT 00:24One must carefully consider the epistemological foundations upon which bioequivalence is predicated. The statistical parameters of 80-125% are not indicative of therapeutic equivalence per se, but rather a pragmatic concession to the ontological limitations of pharmacokinetic measurement. The human organism, as a dynamic and non-linear system, resists reductionist quantification-thus, the very notion of 'sameness' in pharmaceutical absorption is a linguistic construct, not an empirical truth.
Donna Fleetwood
February 3, 2026 AT 00:58Hey everyone, just wanted to say-don’t stress if your generic looks different! I used to panic every time my pill changed color, but my doctor showed me the FDA data and now I’m chill. Generics are heroes. They let people like my mom on fixed income actually afford her meds. 💙