When a bacterial infection reaches the central nervous system-like the brain or spinal cord-it becomes a medical emergency. Infections like bacterial meningitis, brain abscesses, or ventriculitis can kill within hours if not treated fast and right. Tobramycin is one of the antibiotics doctors turn to in these life-or-death moments, especially when other drugs fail. But it’s not a simple pill you pop. It’s a powerful tool with serious risks, used only in hospitals under strict supervision. Here’s what actually happens when tobramycin is used for CNS infections, who it helps, and why it’s not the first choice for most cases.
What Is Tobramycin?
Tobramycin is an tobramycin is an aminoglycoside antibiotic derived from the bacterium Streptomyces tenebrarius. Also known as Tobrex, it was first approved in the 1970s and remains in use today for serious Gram-negative bacterial infections. It works by slipping into bacterial cells and messing up their protein-making machinery, which stops them from multiplying. It’s especially effective against tough bugs like Pseudomonas aeruginosa, Escherichia coli, and Klebsiella pneumoniae-the same ones often behind hospital-acquired CNS infections.
Unlike penicillin or amoxicillin, tobramycin doesn’t cross the blood-brain barrier well on its own. That’s a big problem when you’re trying to treat an infection inside the skull or spine. So doctors don’t give it as a standard IV drip for meningitis. Instead, they use special methods to get it where it needs to go.
How Does Tobramycin Reach the Central Nervous System?
The blood-brain barrier is designed to keep toxins and drugs out of the brain. That’s good for protecting your brain-but terrible when you need antibiotics inside it. Normal IV tobramycin only reaches about 5-10% of the concentration in the brain that it does in the bloodstream. That’s not enough to kill bacteria.
So how do doctors get enough of it in? There are three main ways:
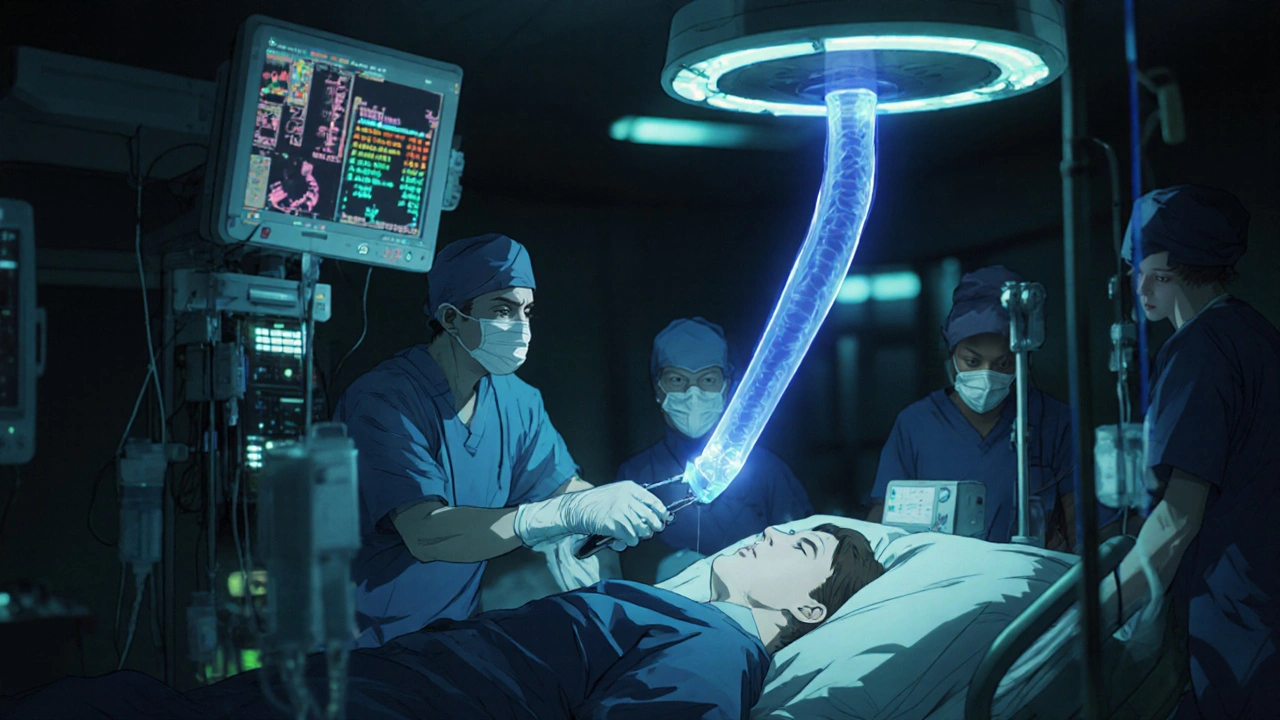
- Intrathecal injection-directly into the spinal fluid via a lumbar puncture. This bypasses the blood-brain barrier completely. Doses are tiny, usually 5-20 mg, and given every 2-3 days. It’s messy, risky, and only done in intensive care units.
- Intraventricular injection-injected directly into the brain’s ventricles through an external drain or Ommaya reservoir. Used for ventriculitis or when the infection is deep inside the brain. Requires a neurosurgical procedure.
- High-dose IV infusion-given in massive doses (up to 12 mg/kg/day) to push more drug across the barrier. This works better when the blood-brain barrier is already damaged by inflammation, which happens in severe meningitis.
Studies from Johns Hopkins and the Mayo Clinic show that combining high-dose IV tobramycin with intrathecal dosing leads to better outcomes than either alone in patients with resistant Pseudomonas meningitis. One 2023 review in Clinical Infectious Diseases found that patients treated with this combo had a 68% survival rate, compared to 41% with standard antibiotics.
When Is Tobramycin Used for CNS Infections?
Tobramycin isn’t used for every CNS infection. It’s reserved for specific, high-risk situations:
- Drug-resistant bacterial meningitis-especially when cultures show Pseudomonas aeruginosa or other multi-drug-resistant Gram-negative bacteria.
- Post-surgical infections-after brain surgery, shunt placement, or trauma where bacteria enter the CNS.
- Failed first-line treatment-when vancomycin, ceftriaxone, or meropenem don’t work.
- Immunocompromised patients-like those on chemotherapy or after organ transplants, who are more vulnerable to rare, aggressive infections.
It’s rarely used in children under 12 unless absolutely necessary. In newborns, it’s sometimes used for neonatal meningitis caused by Gram-negative organisms, but only alongside other antibiotics like ampicillin.
Why Isn’t Tobramycin the First Choice?
There are two big reasons: safety and alternatives.
First, tobramycin is toxic. It can damage your kidneys (nephrotoxicity) and your hearing (ototoxicity). About 10-25% of patients on long-term tobramycin develop some level of hearing loss, and up to 20% show signs of kidney stress. These effects can be permanent. That’s why doctors monitor blood levels constantly-targeting 3-5 mcg/mL for peak levels and under 1 mcg/mL for troughs.
Second, better, safer drugs exist for most cases. Ceftriaxone, cefotaxime, and meropenem cross the blood-brain barrier much better and have fewer side effects. Vancomycin is preferred for Gram-positive infections like MRSA. Tobramycin is a last-line weapon-not a starter pistol.
Real-World Use: A Case Example
In 2024, a 68-year-old man in Melbourne developed fever, confusion, and neck stiffness after a brain tumor resection. His cerebrospinal fluid culture grew Pseudomonas aeruginosa resistant to three antibiotics. He was started on high-dose IV meropenem, but his fever didn’t drop. A repeat spinal tap showed persistent bacteria.
Doctors added intrathecal tobramycin-10 mg every 48 hours-alongside IV tobramycin at 10 mg/kg/day. Within 72 hours, his fever broke. By day 5, his mental status improved. He completed a 14-day course and was discharged with no hearing loss or kidney damage. His case was unusual because he responded so quickly, but it’s not rare in specialized neuro-infectious disease units.
Risks and Side Effects You Can’t Ignore
Even when tobramycin works, it comes at a cost. Here’s what can go wrong:
- Hearing loss-usually starts with high-frequency tones you can’t hear anymore, like birds chirping or doorbells. It can become permanent.
- Kidney damage-signs include less urine output, swelling in the legs, or rising creatinine levels on blood tests.
- Nerve problems-tingling, muscle weakness, or dizziness from nerve toxicity.
- Allergic reactions-rare, but possible: rash, itching, or anaphylaxis.
Patients on tobramycin get daily blood tests for kidney function and weekly hearing checks. If levels go too high, the drug is stopped immediately. No one takes this drug home-it’s strictly hospital-only.
Alternatives to Tobramycin for CNS Infections
Doctors don’t want to use tobramycin if they don’t have to. Here’s what they try first:
| Antibiotic | Best For | CSF Penetration | Key Risks |
|---|---|---|---|
| Ceftriaxone | Common meningitis (Strep, N. meningitidis) | High (80-100%) | Diarrhea, allergic reactions |
| Meropenem | Drug-resistant Gram-negative, post-op infections | High (70-90%) | Seizures (rare), GI upset |
| Vancomycin | MRSA, Gram-positive infections | Moderate (30-50%) | Kidney damage, red man syndrome |
| Aztreonam | Pseudomonas in penicillin-allergic patients | Moderate (40-60%) | Minimal kidney toxicity |
| Tobramycin | Resistant Pseudomonas, last-resort | Low (5-10%) without direct delivery | Hearing loss, kidney damage |
Aztreonam is gaining traction as a safer alternative for Gram-negative infections in patients who can’t take beta-lactams. But it’s not as potent against some strains of Pseudomonas as tobramycin.
What Patients and Families Should Ask
If you or a loved one is being considered for tobramycin treatment, here are five critical questions to ask:
- Is this infection confirmed to be caused by a bacteria that tobramycin can kill?
- Have we tried other antibiotics first? Why didn’t they work?
- Will you be giving tobramycin through the spine or brain, or just IV?
- How often will you check my hearing and kidney function?
- What happens if I lose my hearing or my kidneys are damaged?
There’s no shame in asking. This is a high-risk treatment. You deserve to know why it’s being used and what the trade-offs are.
Final Thoughts: A Tool, Not a Cure-All
Tobramycin saves lives-but it doesn’t come without scars. It’s not a miracle drug. It’s a scalpel used only when the infection is too dangerous to cut with anything else. Its use in CNS infections is rare, precise, and tightly controlled. For most people, safer, more effective antibiotics will do the job. But when the bacteria are resistant, the brain is under attack, and time is running out-tobramycin might be the only thing standing between life and death.
If you’re facing this situation, trust your medical team-but don’t stop asking questions. The right antibiotic, given the right way, at the right time, can change everything.
Can tobramycin cure viral meningitis?
No. Tobramycin only works against bacteria. Viral meningitis is caused by viruses like enteroviruses, and antibiotics have no effect. Treatment is supportive-rest, fluids, and pain relief. Using tobramycin for viral meningitis is unnecessary and risky.
Is tobramycin safe for children?
It’s used in children only in extreme cases, like neonatal meningitis caused by resistant Gram-negative bacteria. Dosing is based on weight and kidney function, and monitoring is even stricter than in adults. Hearing tests are done before, during, and after treatment. Most pediatric infectious disease specialists avoid it unless there are no other options.
Can you take tobramycin by mouth for a CNS infection?
No. Oral tobramycin isn’t absorbed into the bloodstream at all-it stays in the gut. That’s why it’s used for gut infections like those caused by E. coli in travelers’ diarrhea. For CNS infections, it must be delivered directly into the spinal fluid or given in massive IV doses.
How long does tobramycin treatment last for CNS infections?
Typically 10 to 21 days, depending on the infection type and how well the patient responds. For meningitis, treatment often continues for at least 14 days after symptoms improve and cultures turn negative. Brain abscesses may need 4-6 weeks. Stopping too early risks relapse.
Does tobramycin interact with other medications?
Yes. It can worsen kidney damage when used with other nephrotoxic drugs like vancomycin, NSAIDs, or contrast dyes. It can also increase the risk of muscle weakness when combined with neuromuscular blockers used during surgery. Always tell your doctor about every medication you’re taking, including supplements.

 Medications
Medications
Holly Dorger
October 31, 2025 AT 05:07tobramycin sounds like something out of a sci-fi movie where the doctor has to inject it straight into your spine like a superhero serum. i had no idea it was this intense. my uncle got it after brain surgery and he lost some high-pitched hearing but survived. worth it? i dont know. but i’m glad they had it.
Amanda Nicolson
November 1, 2025 AT 09:41okay but imagine being the nurse who has to prepare this stuff. one wrong milligram and someone’s hearing is gone forever. i work in oncology and we use chemo that’s brutal but at least we know the side effects are predictable. tobramycin feels like playing russian roulette with a patient’s senses. and yet-when there’s no other choice? it’s the only thing holding the line between life and a coma. i’m in awe of the doctors who use it. and terrified of ever needing it.
Jackson Olsen
November 1, 2025 AT 19:51Penny Clark
November 3, 2025 AT 05:42i read this whole thing with my heart in my throat. my cousin was in the icu with pseudomonas meningitis after a car accident. they used tobramycin intrathecally and she woke up after 10 days. no hearing loss, no kidney issues. it felt like a miracle. but the doctors said it was luck-the right dose, the right timing, the right team. this drug isn’t magic. it’s a gamble. and the people who use it? they’re the quiet heroes.
Niki Tiki
November 4, 2025 AT 09:15Jim Allen
November 4, 2025 AT 21:16so basically tobramycin is the last resort because everything else failed. so why not just start with it? save time. save money. save lives. why play nice with ceftriaxone when you can just go nuclear from the start? i get the side effects but if your brain is being eaten by bacteria, who cares if you can’t hear birds anymore? you’re alive. and birds can still chirp for your kids.
Nate Girard
November 5, 2025 AT 22:40thank you for writing this. i’m a med student and this is exactly the kind of info we don’t get in lectures-real-world use, trade-offs, the human cost. i had a rotation in neurology last month and saw a patient on intrathecal tobramycin. she was 22, terrified, and asked if she’d ever hear her mom’s voice again. we didn’t know the answer. but we gave her the drug anyway. this post made me feel less alone in that moment.
Carolyn Kiger
November 6, 2025 AT 00:44the part about aztreonam as a safer alternative really stood out to me. i’ve got a friend with cystic fibrosis who’s on it for lung infections and she says it’s way gentler than tobramycin. if it works for pseudomonas in the lungs, why not push for more research on using it for CNS? maybe we don’t need to risk hearing loss if there’s a gentler path. we should be investing in alternatives-not just pushing the same old scalpel harder.