HIV Medication & Birth Control Interaction Checker
Check Your Birth Control Safety
Select your HIV medication and birth control method to see if your contraception is still effective.
When you’re managing HIV with antiretroviral therapy, your life already involves a careful balance of medications, appointments, and daily routines. Now add birth control to the mix - and suddenly, something as simple as taking the pill becomes a high-stakes decision. The truth? HIV protease inhibitors can seriously reduce the effectiveness of many hormonal contraceptives. This isn’t a rare side effect. It’s a well-documented, clinically significant interaction that has led to unplanned pregnancies, delayed care, and heartbreaking choices for women around the world.
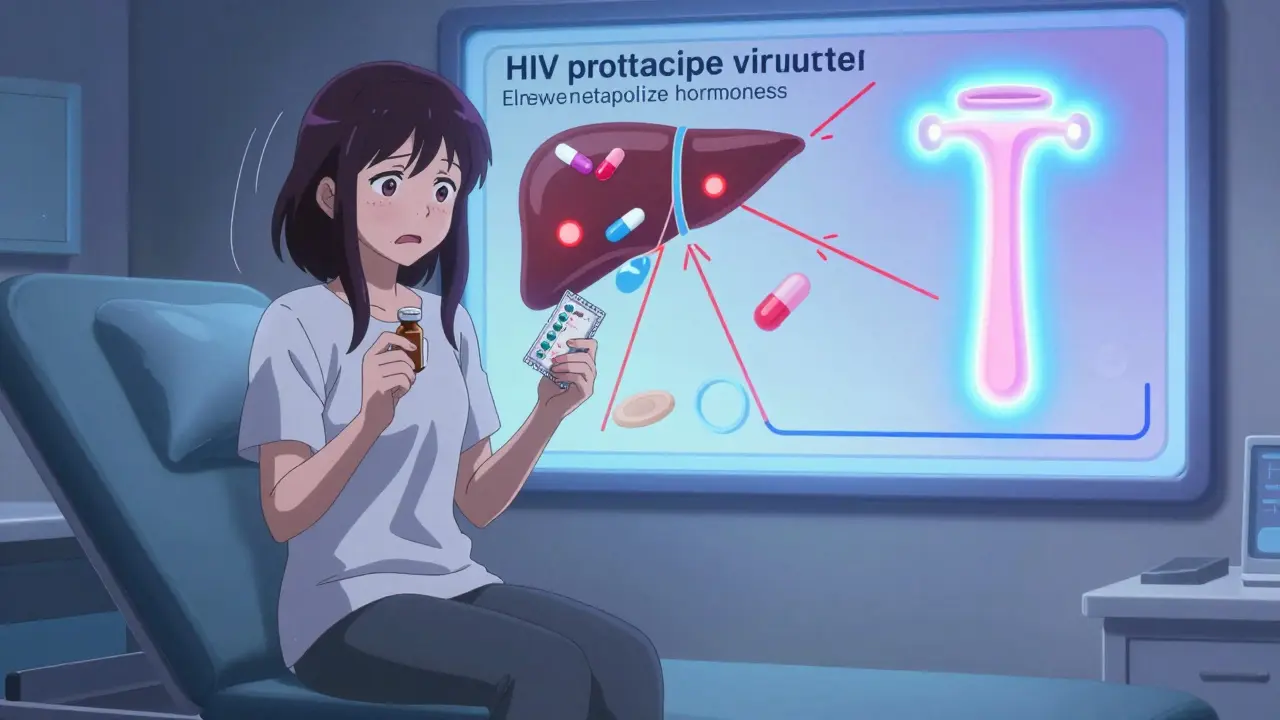
How HIV Medications Break Down Birth Control
HIV protease inhibitors - like lopinavir, atazanavir, and darunavir - don’t just fight the virus. They also mess with your body’s ability to process hormones. These drugs are metabolized through the same liver enzyme system - CYP3A4 - that breaks down estrogen and progestin in birth control pills, patches, rings, and even implants. When protease inhibitors are in your system, they can either block or speed up this process, leaving you with too little or too much hormone circulating in your blood.It’s not just about feeling different - it’s about whether your body has enough of the right hormone to stop ovulation. Studies show that when women take lopinavir/ritonavir with the contraceptive patch, ethinyl estradiol levels drop by 45%. That’s not a small dip. That’s falling below the threshold needed to prevent pregnancy. In another study, women using the hormonal ring (NuvaRing) with efavirenz had subtherapeutic levels of etonogestrel in 38% of cases. That means, for nearly four in ten women, the ring was doing nothing to prevent pregnancy - even if they used it perfectly.
Which Birth Control Methods Are Riskiest?
Not all hormonal contraceptives are created equal when it comes to drug interactions. Some are more vulnerable than others.- Combined oral contraceptives (COCs): These pills, like Tri-Sprintec or Yaz, contain estrogen and progestin. They’re the most commonly used method - and the most likely to fail when paired with protease inhibitors. Pregnancy rates jump from the usual 7-8% to 11-15% in women taking efavirenz-based regimens.
- Contraceptive patch and ring: These deliver hormones through the skin or vagina, but they’re just as affected. The patch’s ethinyl estradiol levels drop by nearly half with lopinavir/ritonavir. The ring? Same story.
- Progestin-only pills (POPs): Often called the “mini-pill,” these are sometimes thought to be safer. They’re not. The WHO classifies their use with ritonavir-boosted protease inhibitors as Category 3 - meaning the risks usually outweigh the benefits. Even perfect use isn’t enough to guarantee protection.
- Implants and injections: Etonogestrel implants (like Nexplanon) can lose up to 60% of their hormone levels when taken with ritonavir-boosted drugs. Depo-Provera (DMPA) is more stable - but even then, pregnancy rates climb to 12.3 per 100 woman-years with efavirenz, compared to 5.7 with nevirapine.
The pattern is clear: if your birth control relies on steady hormone levels, and you’re on a protease inhibitor - especially one boosted by ritonavir - you’re at risk.
What Works Instead?
The good news? There are options that don’t rely on your liver enzymes. And they’re not just theoretical - they’re proven.- Intrauterine devices (IUDs): Both copper and hormonal IUDs work locally in the uterus. They’re not affected by liver metabolism. Their effectiveness stays at 99%, no matter what HIV meds you’re on. That’s why experts now call them the gold standard for women on antiretrovirals.
- Contraceptive implants (with caveats): If you’re on dolutegravir - now the most common first-line HIV treatment - implants are safe. But if you’re on ritonavir-boosted drugs? Avoid them. The hormone drop is too steep.
- Depot medroxyprogesterone acetate (DMPA): This injection is still considered safe with non-ritonavir-boosted regimens. But with efavirenz? Use with caution. The data is mixed, and pregnancy rates rise.
There’s one more thing: emergency contraception. Levonorgestrel pills (Plan B) may not work as well if you’re on darunavir/cobicistat. Studies show levonorgestrel levels drop by 35%. That means if you need emergency contraception, you might need a higher dose - or a copper IUD inserted within five days.
Real Stories, Real Consequences
Behind the numbers are real people. On HIV support forums, women share stories that don’t show up in clinical trials.One woman, MariaJ, took Tri-Sprintec daily with darunavir/cobicistat. She had no missed pills, no vomiting, no diarrhea. Still, she became pregnant. Her provider confirmed the interaction was likely the cause.
Another, posting on Reddit, used Depo-Provera with atazanavir/ritonavir. She didn’t know about the interaction. At 18 weeks pregnant, she learned the truth: her provider had never mentioned it.
A 2021 survey of 327 HIV-positive women found that 28% had experienced contraceptive failure. Of those, 63% were on protease inhibitors. That’s nearly two out of every three women who got pregnant while using hormonal birth control - not because they were careless, but because they weren’t warned.
Why This Keeps Happening
You’d think this would be common knowledge. But it’s not.A 2018 report from the AIDS Clinical Trials Group found that 41% of women received no counseling about drug interactions when first diagnosed with HIV. Community clinics were even worse - 28% less likely than academic centers to provide this info.
Why? Time. Training. Misunderstanding. Many providers assume birth control is “just birth control.” They don’t realize that HIV meds can turn a 99% effective method into a 60% one. Others think, “She’s on the pill - she knows how to use it.” But the problem isn’t adherence. It’s pharmacology.
Even the labels on birth control boxes don’t always spell it out clearly. The FDA required updated warnings in 2016 - but many women still don’t see them. And in low-resource settings, where access to IUDs is limited, women are forced to choose between HIV treatment and reliable contraception.
What Providers Should Do
The solution isn’t complicated - it’s consistent.- Screen every woman of reproductive age for contraceptive use at every HIV visit.
- Use the CDC’s free online interaction checker - it has 147 drug pairs mapped out.
- Recommend IUDs or implants (if compatible) as first-line options.
- Use the teach-back method: “Tell me in your own words what you’ll use instead.” Studies show this increases understanding from 42% to 85%.
- Train staff. The CDC’s 2-hour online course has trained over 8,000 providers globally - and improved test scores from 64% to 92%.
There’s no excuse for missing this. We have the tools. We have the data. We just need to use them.
The Future Is Changing - But Not Fast Enough
The tide is turning. Dolutegravir, a newer HIV drug, has minimal interaction with birth control. As of 2023, 72% of new HIV patients start on dolutegravir-based regimens. That’s good news - because it means fewer women will face this dilemma in the future.But millions are still on older regimens. And in places where dolutegravir isn’t available, women are still choosing between their health and their fertility. The WHO is now pushing for integrated “one-stop-shop” clinics that combine HIV care and contraception by 2030. That’s the goal. But right now, too many women are falling through the cracks.
The message is simple: if you’re on HIV protease inhibitors - especially ritonavir-boosted ones - don’t rely on pills, patches, or rings. Talk to your provider. Get an IUD. Consider an implant - but only if your HIV meds allow it. Your body is doing enough. Don’t let a hidden drug interaction put your future at risk.
Can I still use the pill if I’m on HIV protease inhibitors?
No - not safely. Combined oral contraceptives (COCs) and progestin-only pills (POPs) are significantly less effective when taken with protease inhibitors like lopinavir, atazanavir, or darunavir. Studies show hormone levels drop by up to 83%, making pregnancy likely even with perfect use. The WHO and CDC classify this combination as high-risk. Switch to an IUD or implant instead.
Are IUDs safe with HIV medications?
Yes - both copper and hormonal IUDs are safe and highly effective, no matter what HIV meds you’re taking. They work locally in the uterus and don’t rely on liver metabolism. Their effectiveness stays at 99%, even with protease inhibitors. They’re the top-recommended option for women on antiretroviral therapy.
What about the birth control implant (Nexplanon)?
It depends on your HIV regimen. If you’re on dolutegravir or raltegravir, the implant is safe and effective. But if you’re on ritonavir-boosted protease inhibitors, hormone levels can drop by 40-60%, making it unreliable. The International AIDS Society-USA advises against using implants with these drugs. Talk to your provider about your specific meds before choosing this option.
Can I use emergency contraception if I’m on HIV meds?
Levonorgestrel emergency pills (like Plan B) may be less effective if you’re on darunavir/cobicistat - studies show a 35% drop in hormone levels. Your best bet is a copper IUD inserted within five days, which is over 99% effective as emergency contraception. If you must use a pill, consider a higher dose (1.5 mg) and follow up with a pregnancy test if your period is late.
Why don’t more doctors warn women about this?
Many don’t know. A 2018 study found 41% of women received no counseling about these interactions at their HIV diagnosis. Community clinics are especially likely to overlook this. Training is improving - the CDC’s online course has trained over 8,000 providers - but gaps remain. If your provider hasn’t brought it up, ask. Your safety depends on it.
What to Do Next
If you’re on HIV protease inhibitors and using hormonal birth control:- Check your HIV meds. Are you on ritonavir, cobicistat, lopinavir, atazanavir, or darunavir? If yes, your birth control may not be working.
- Don’t stop your HIV meds. That’s dangerous. Instead, talk to your provider about switching your contraception.
- Ask for an IUD. It’s the most reliable, long-term solution.
- Use the CDC’s free online interaction checker to confirm your specific drug combo.
- If you’ve had an unplanned pregnancy, know you’re not alone - and you’re not to blame.
This isn’t about fear. It’s about facts. And the facts are clear: if you’re on protease inhibitors, your birth control may be failing - and you deserve better.

 Medications
Medications
Aysha Siera
January 16, 2026 AT 16:13Wendy Claughton
January 17, 2026 AT 16:19Stacey Marsengill
January 18, 2026 AT 23:15Robert Davis
January 20, 2026 AT 17:26Eric Gebeke
January 21, 2026 AT 23:47Jake Moore
January 22, 2026 AT 08:13Joni O
January 22, 2026 AT 14:19Ryan Otto
January 24, 2026 AT 13:19Max Sinclair
January 25, 2026 AT 05:00Praseetha Pn
January 25, 2026 AT 10:54