Trying to get pregnant? If you’ve been trying for months without success, it’s easy to blame stress, age, or bad luck. But there’s one often-overlooked factor that could be quietly holding you back: your thyroid.
Why Thyroid Health Matters Before Pregnancy
Your thyroid isn’t just about energy or weight. It’s a master regulator of your metabolism, hormones, and reproductive system. Even small imbalances can interfere with ovulation, disrupt menstrual cycles, and lower your chances of getting pregnant. And once you do conceive, your thyroid has to work harder-sometimes up to 50% harder-to support your growing baby, especially in the first trimester when the fetus can’t make its own thyroid hormone.Studies show that women with untreated or poorly managed thyroid conditions have higher rates of miscarriage, preterm birth, and developmental issues in their babies. The good news? Thyroid problems are one of the most treatable causes of infertility. Fix your TSH levels before conception, and you dramatically improve your odds.
What Is TSH, and Why Does It Matter?
TSH stands for Thyroid-Stimulating Hormone. It’s made by your pituitary gland and tells your thyroid how much hormone to produce. When TSH is high, your thyroid isn’t making enough. When it’s low, you might be making too much.For most adults, a normal TSH range is 0.4 to 4.0 mIU/L. But that’s not the right target if you’re trying to get pregnant. Research from the American Thyroid Association (ATA) shows that women aiming for pregnancy should aim for a TSH level below 2.5 mIU/L before conceiving. Why? Because even TSH levels between 2.5 and 4.0-still technically "normal"-are linked to lower pregnancy rates and higher miscarriage risk.
A 2018 study of over 7,000 women found that nearly twice as many women with unexplained infertility had TSH levels ≥2.5 mIU/L compared to women who conceived easily. Another large analysis of 180,000 pregnancies showed women with TSH above 2.5 had a 15% higher risk of miscarriage.
What If You Have Hashimoto’s or Thyroid Antibodies?
If you’ve been diagnosed with Hashimoto’s thyroiditis-or your blood tests show thyroid antibodies (TPOAb or TgAb)-your needs are even more specific. Your immune system is already attacking your thyroid. Pregnancy adds extra stress, and your thyroid may struggle to keep up.Experts now recommend that women with thyroid autoimmunity aim for an even lower TSH target: between 1.25 and 1.75 mIU/L before conception. Why? Because during early pregnancy, your body’s demand for thyroid hormone spikes, and if your thyroid is already compromised, it won’t be able to respond fast enough. This can lead to early pregnancy loss or developmental delays in the baby.
Even if your TSH is normal but you have antibodies, your risk of miscarriage is still higher. Pooled data from multiple studies show that taking levothyroxine (the standard thyroid medication) can reduce miscarriage risk by 45% and improve live birth rates by 36% in these women.
What About Women With Normal TSH But No Diagnosis?
This is where things get messy. Some doctors won’t test your thyroid unless you have obvious symptoms-fatigue, weight gain, hair loss, irregular periods. But many women with subclinical hypothyroidism feel fine. They just can’t get pregnant.The American Society for Reproductive Medicine (ASRM) recommends screening all women undergoing fertility evaluation for TSH. Why? Because about 15-20% of women with unexplained infertility have abnormal TSH levels. And most of them don’t even know it.
If your TSH is between 2.5 and 4.0 and you’re trying to conceive, don’t wait. Get a full thyroid panel: TSH, free T4, and thyroid antibodies. If your TSH is above 2.5, even if you feel fine, it’s worth talking to your doctor about starting low-dose levothyroxine. It’s safe, cheap (as little as $4 a month), and could be the missing piece.
Levothyroxine: The Right Medication, the Right Way
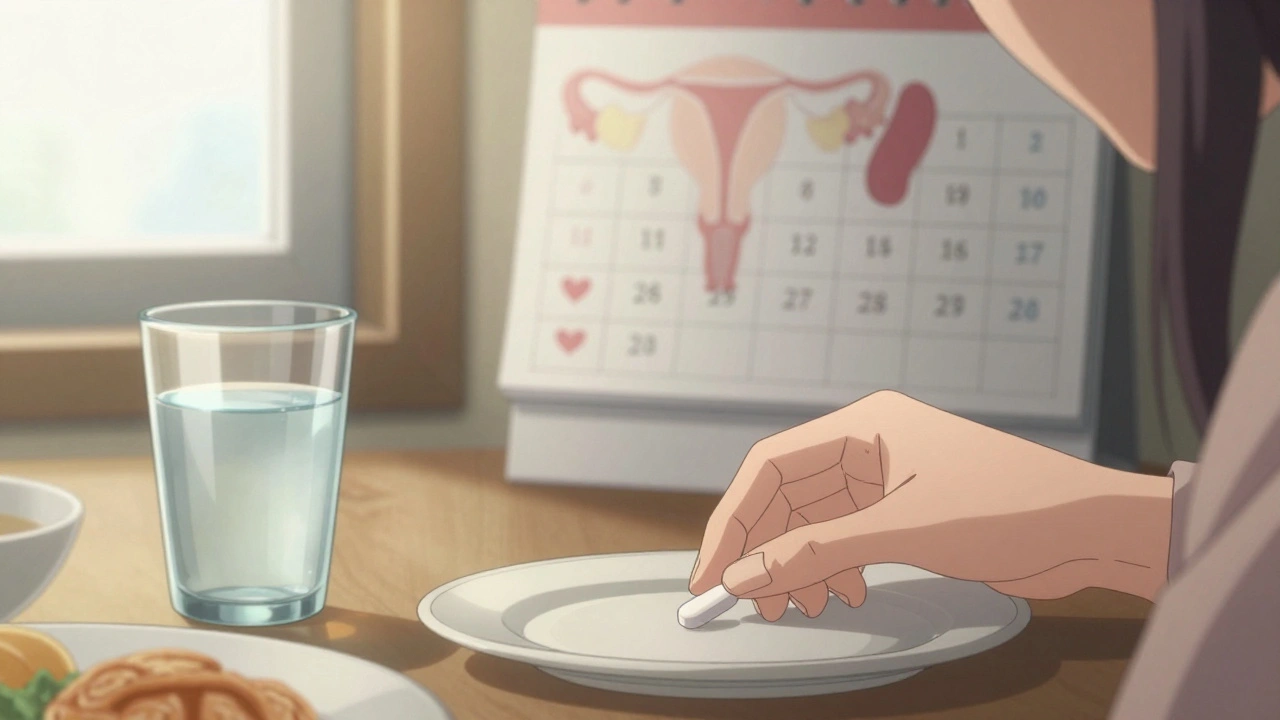
Levothyroxine is the only thyroid medication recommended before and during pregnancy. It’s a synthetic version of T4, the main hormone your thyroid makes. It’s stable, predictable, and doesn’t cross the placenta in harmful amounts.Avoid desiccated thyroid (like Armour Thyroid). These are made from pig thyroid glands and contain both T3 and T4. They’re inconsistent in dose and can cause dangerous swings in hormone levels. InVia Fertility Center and other leading clinics specifically warn against using them during preconception or pregnancy.
When you start levothyroxine, take it on an empty stomach-first thing in the morning, with a full glass of water. Wait at least 30 minutes before eating or drinking anything else. Avoid calcium, iron, or antacids within four hours of your dose. These minerals bind to the medication and block absorption.
Once you get pregnant, your dose will likely need to go up by 25-50%. Many women don’t realize this. A 2019 study found that only 37% of women with hypothyroidism had their dose adjusted after conception. That’s too late. Your baby’s brain development depends on your thyroid hormone in the first 12 weeks. Waiting until your next appointment could mean missing a critical window.
How Often Should You Get Tested?
If you’re trying to conceive and have thyroid issues, don’t wait six months for a checkup. Test your TSH every 4 to 6 weeks until your level is consistently below 2.5 mIU/L. Once you’re pregnant, test every 4 weeks through the first half of pregnancy. After that, you can space out tests unless your doctor advises otherwise.Don’t rely on just TSH. Ask for free T4 too. Some women have normal TSH but low T4, which means their thyroid isn’t producing enough active hormone. That’s just as dangerous.
What If Your TSH Is Below 0.1? (Hyperthyroidism)
High TSH means underactive thyroid. But low TSH (below 0.1) means overactive thyroid-hyperthyroidism. That’s also bad for fertility and pregnancy. It can cause irregular periods, weight loss, rapid heartbeat, and increase the risk of preterm birth and preeclampsia.If you have Graves’ disease or another cause of hyperthyroidism, get it under control before trying to conceive. Medications like methimazole are safe during pregnancy, but radioactive iodine treatment is not. If you’ve had that treatment, wait at least six months before trying to get pregnant.
Cost vs. Benefit: Why This Isn’t Just "Nice to Do"
Levothyroxine costs about $4 to $10 a month. A single miscarriage, by comparison, can cost over $7,200 in medical care, lost wages, and emotional toll. Preconception thyroid screening and treatment saves an estimated $1,850 to $2,400 per pregnancy by reducing miscarriages and preterm births.And it’s not just money. It’s peace of mind. Knowing you’ve done everything you can to give your baby the best start is priceless.
What’s Changing in 2025?
Guidelines are evolving. The European Thyroid Association now recommends even stricter targets: TSH under 1.8 mIU/L in the first 4 weeks after conception, rising slightly to 2.8 mIU/L by week 12. The American Thyroid Association is reviewing new data and may update its guidelines soon.A major NIH-funded trial (NCT03856002) is wrapping up in late 2024. Early results suggest personalized TSH targets-based on your antibody status and thyroid reserve-might work better than a one-size-fits-all 2.5 mIU/L cutoff. But until those results are published, the safest bet remains: aim for under 2.5.
What You Can Do Today
- If you’re trying to conceive and haven’t had your thyroid checked in the last year, ask your doctor for a TSH test. Request free T4 and thyroid antibodies too.
- If your TSH is above 2.5, don’t wait. Talk to an endocrinologist or reproductive specialist about starting levothyroxine.
- If you already take levothyroxine, get your levels checked now-not when you get a positive pregnancy test.
- Take your medication correctly: empty stomach, water only, wait 30 minutes before eating.
- Avoid calcium, iron, and antacids within 4 hours of your dose.
- Once pregnant, schedule your next TSH test within 4 weeks. Don’t assume your old dose is still enough.
Thyroid health isn’t a luxury. It’s a foundation. For your fertility. For your pregnancy. For your baby’s future. Don’t wait until it’s too late. Get tested. Get treated. Get ready.
Can low thyroid function cause infertility?
Yes. Low thyroid function (hypothyroidism) can disrupt ovulation, cause irregular periods, and increase prolactin levels, which suppresses fertility. Even mild cases with TSH above 2.5 mIU/L are linked to lower pregnancy rates and higher miscarriage risk. Treating it with levothyroxine often restores fertility.
Should I get my TSH tested if I’m not having trouble getting pregnant?
If you’re planning to conceive in the next 6-12 months, yes. Many women with thyroid issues feel fine until they try to get pregnant. The American Society for Reproductive Medicine recommends TSH screening for all women starting fertility evaluation. Even if you’re not yet trying, testing now gives you time to optimize your levels before conception.
Is it safe to take levothyroxine while trying to conceive?
Yes. Levothyroxine is a synthetic version of the natural thyroid hormone your body makes. It’s safe during preconception and pregnancy. In fact, it’s safer than untreated hypothyroidism. The goal is to mimic your body’s normal hormone levels-not overcorrect or undercorrect. Always use levothyroxine, not natural thyroid extracts like Armour Thyroid.
How long does it take for TSH to stabilize after starting or changing levothyroxine?
It takes about 4 to 6 weeks for your body to fully adjust to a new dose. That’s why doctors test TSH every 4-6 weeks during preconception optimization. Don’t rush. Small, steady adjustments are safer and more effective than large, sudden changes.
Can I stop taking levothyroxine after I get pregnant?
No. Your body’s need for thyroid hormone increases during pregnancy-often by 30-50%. Stopping or skipping doses can harm your baby’s brain development, especially in the first trimester. Most women need to increase their dose after conception. Never stop without consulting your doctor.
What if my TSH is normal but I have thyroid antibodies?
Even with normal TSH, thyroid antibodies (like TPOAb) increase your risk of miscarriage by about 2-fold. Studies show that taking low-dose levothyroxine can reduce this risk by 45%. If you have antibodies and are trying to conceive, ask your doctor about starting treatment-even if your TSH is in the "normal" range.
For more information, refer to guidelines from the American Thyroid Association, American Society for Reproductive Medicine, and the Endocrine Society. Always work with a healthcare provider who understands the link between thyroid health and fertility.


 Medications
Medications
Yasmine Hajar
December 4, 2025 AT 23:03I was told my TSH was 'fine' at 3.2 until I hit 3 miscarriages in 2 years. My RE finally ordered a full panel and found my antibodies were through the roof. Started levothyroxine at 25mcg and got pregnant within 3 months. No more 'normal' ranges for fertility-2.5 is the new 4.0. Thank you for this post.
Karl Barrett
December 5, 2025 AT 05:03From a neuroendocrinological standpoint, the pituitary-thyroid-ovarian axis is a tightly coupled feedback loop. Subclinical hypothyroidism elevates prolactin via TRH upregulation, which directly inhibits GnRH pulsatility. The 2.5 mIU/L threshold isn’t arbitrary-it’s the point where T4-to-T3 conversion in the follicular fluid becomes insufficient for oocyte maturation. Levothyroxine isn’t just replacement-it’s neuroendocrine normalization.
Jake Deeds
December 5, 2025 AT 23:42Wow. So now we’re supposed to be paranoid about our thyroid levels before we even try? I mean, I get it, but isn’t this just another way doctors make money? I’m just saying-maybe we should stop medicalizing everything. I got pregnant naturally at 38 with a TSH of 3.8. My kid’s a genius. Maybe the real issue is anxiety?
val kendra
December 6, 2025 AT 15:19Just got my labs back-TSH 3.1, TPOAb high. Doctor said ‘wait and see.’ I said nope. Went to an endo, started 25mcg levothyroxine. 6 weeks later-TSH 1.9. Trying next cycle. If you’re trying and your TSH is above 2.5, don’t wait. It’s not ‘maybe.’ It’s ‘do it now.’ And take it on an empty stomach. No coffee. No calcium. No excuses.
Also-stop scrolling. Go book your blood test.
Isabelle Bujold
December 8, 2025 AT 10:24I’ve been working as a reproductive endocrinology nurse for over 15 years and I can’t tell you how many women I’ve seen who were told their thyroid was ‘fine’-only to find out later that their TSH was 3.7 and their free T4 was borderline low. The standard lab range is based on the general population, not women trying to conceive. That’s like saying your blood pressure is fine because it’s under 140/90 when you’re pregnant. The real target is 1.5–2.5, and if you have antibodies, even lower. I’ve watched women cry because they didn’t know this until after their third loss. Please, if you’re reading this and you’re trying-get tested. It’s a simple blood draw. It could change everything.
George Graham
December 8, 2025 AT 17:42This is the kind of post that saves lives. I didn’t know anything about thyroid and fertility until my wife had her second miscarriage. We were devastated. Then we found this exact info. She got tested, started meds, and now we’re 14 weeks pregnant. I never realized how much this invisible hormone could affect everything. Thank you for sharing the science, not just the fear.
John Filby
December 9, 2025 AT 15:19Just started levothyroxine last week after my TSH came back at 3.4. Took me 8 months to get my doctor to test. So glad I didn’t give up. Also-yes, take it on an empty stomach. I forgot once and had coffee 20 mins later… felt like my brain was in a fog for 3 hours. 🤦♀️
Also, side note: my period came back on time for the first time in 2 years. Wild.
Elizabeth Crutchfield
December 10, 2025 AT 03:39i had no symptoms just couldnt get preggo and my tsh was 3.9… doc said its fine… i went private and got meds… got pregnant in 2 months… dont wait for symptoms… test now
Ben Choy
December 11, 2025 AT 02:38Just wanted to add-my TSH was 1.8 when I conceived, but after I got pregnant, they didn’t bump my dose until 10 weeks. Turned out my free T4 was dropping. Baby’s fine now, but I wish I’d known to push for weekly checks in the first trimester. This post is gold. Please share it with every woman you know who’s TTC.
Emmanuel Peter
December 12, 2025 AT 06:16Wait, so if your TSH is above 2.5, you’re basically a bad mom already? You’re saying women who don’t get tested are irresponsible? What if they can’t afford it? What if they don’t have access to a doctor? This post feels like guilt-tripping people who are already stressed enough. Maybe the real problem is healthcare inequality, not their thyroid levels.