When a critical medication expires, it’s not just a paperwork issue-it’s a patient safety emergency. In hospitals, ICUs, and even some long-term care facilities, an expired drug like fentanyl, midazolam, or norepinephrine can mean the difference between life and death. But you can’t just grab the next similar-looking pill from the shelf. You need a system. A clear, evidence-based way to decide what to use instead. And if you’re working in a hospital without one, you’re already behind.
Why Expired Medications Are Different from Shortages
Most people think expired meds and drug shortages are the same thing. They’re not. A shortage means the drug isn’t being made or shipped. An expired medication means it was there, but time ran out. The key difference? Expired drugs are often still physically present-just unusable. That means you have to replace them fast, with no time to wait for new shipments. In the ICU, patients are on 5 to 10 medications at once. One expired sedative? That could trigger withdrawal. One expired vasopressor? Blood pressure crashes. And if you guess wrong? You could cause organ failure, seizures, or cardiac arrest. This isn’t theoretical. In 2024, a study of 10,000 ICU cases found that when replacement protocols weren’t followed, medication errors led to 18.7% higher mortality rates.The Three-Tier Replacement System (ASHP Standard)
The American Society of Health-System Pharmacists (ASHP) has a proven framework for this exact problem. It’s called the three-tier system. It’s not a suggestion. It’s the gold standard used in 89% of academic medical centers. Here’s how it works:- 1st Line: Direct Therapeutic Equivalent - The exact same drug class, same mechanism, same dosing profile. For example, if your fentanyl infusion expires, hydromorphone is a 1st line replacement. It’s not identical, but it’s predictable. Dose conversion is well-documented.
- 2nd Line: Clinically Valid Alternative - A drug that works similarly but has different kinetics. Like switching from cisatracurium to rocuronium for neuromuscular blockade. You’ll need to adjust the dose, monitor longer, and watch for side effects.
- 3rd Line: Last Resort - Only if 1st and 2nd aren’t available. Maybe you’re forced to use vecuronium when rocuronium is out. It’s not ideal. It’s slower, harder to reverse. But it’s better than nothing.
How to Implement a Replacement Protocol in 7 Steps
You don’t need a big budget. You need structure. Here’s how to build one, even if you’re the only pharmacist on duty:- Validate the expiration - Don’t assume. Check the lot number, expiration date, and quantity. Was it stored correctly? Was it exposed to heat or light? Sometimes a drug looks expired but is still stable. The FDA’s 2025 draft guidance on shelf-life extension may soon make this easier, but for now, stick to the label.
- Count remaining stock - How much is left? Is it enough for one dose? Ten? If it’s 200 mL of something that lasts 48 hours, you have time. If it’s 10 mL? You’re in crisis mode.
- Identify affected patients - Who’s on this drug? How many? Are they ventilated? On dialysis? Kidney failure? This changes everything. A drug that’s safe for a healthy 30-year-old might kill someone with liver disease.
- Match to tiered alternatives - Pull up your ASHP protocol. Use the 1st line first. If you can’t get it, move to 2nd. Never skip tiers unless you’re out of options. Document why.
- Adjust doses - This is where mistakes happen. Fentanyl to hydromorphone isn’t 1:1. It’s roughly 1:10. Get it wrong, and you overdose or underdose. Always use a trusted conversion chart. Never rely on memory.
- Update the EHR and barcodes - If the system still shows fentanyl as active, someone will order it again. Change the inventory record. Flag the new drug in the order set. This step is often skipped-and it’s why errors repeat.
- Monitor and document - For the next 72 hours, track vital signs, sedation scores (RASS), and lab values. If the patient’s heart rate spikes or they start shivering, you might be seeing withdrawal. Log everything. This isn’t bureaucracy. It’s your legal protection.
Who Should Be on the Replacement Team?
This isn’t a pharmacist’s job alone. It’s a team sport. In high-performing hospitals, there’s a daily medication safety huddle-15 minutes, before rounds. Pharmacists, nurses, intensivists, and sometimes even respiratory therapists gather. They review: expired meds, upcoming expirations, pending orders, and any last-minute changes. Why does this work? Because nurses see the patient 12 times a day. They notice when someone’s restless. Pharmacists know the drugs. Doctors know the diagnosis. Together, they catch what no one person would see alone. In community hospitals? Only 42% have this. That’s why they have 3x more medication errors. If your hospital doesn’t have this, start it. Even if it’s just you and one nurse, meeting every morning. It changes outcomes.What Happens When You Don’t Have a Protocol?
In 2024, a Reddit post from an ICU nurse in rural Ohio went viral. Her hospital’s fentanyl expired. No pharmacist on site. No written guidelines. The team tried switching to morphine. Then to tramadol. Then to acetaminophen. The patient went into withdrawal. Had a seizure. Ended up in the ER again 11 days later. That’s not rare. The National Critical Care Survey found that hospitals without formal replacement protocols had 32% more medication-related readmissions. And those readmissions cost an average of $11,200 per patient. The worst part? Many of these errors are preventable. You don’t need AI. You don’t need a million-dollar system. You need a printed sheet with the three-tier list taped to the pharmacy counter.Technology Can Help-But It’s Not a Fix
Some hospitals use automated systems that alert them 30 days before a drug expires. Others use barcode scanning to block expired meds from being dispensed. AI tools are now being tested that analyze 147 patient factors-like kidney function, age, and current sedation level-to recommend the best replacement. But here’s the truth: technology doesn’t replace judgment. It supports it. A 2025 study at CU Anschutz found that AI-recommended replacements matched expert pharmacists 94.7% of the time. But when the AI was used without a pharmacist present? Errors doubled. Why? Because the AI didn’t know the patient’s history. It didn’t know the nurse had already seen withdrawal signs. It didn’t know the family had refused certain drugs. So use tech. But never trust it alone.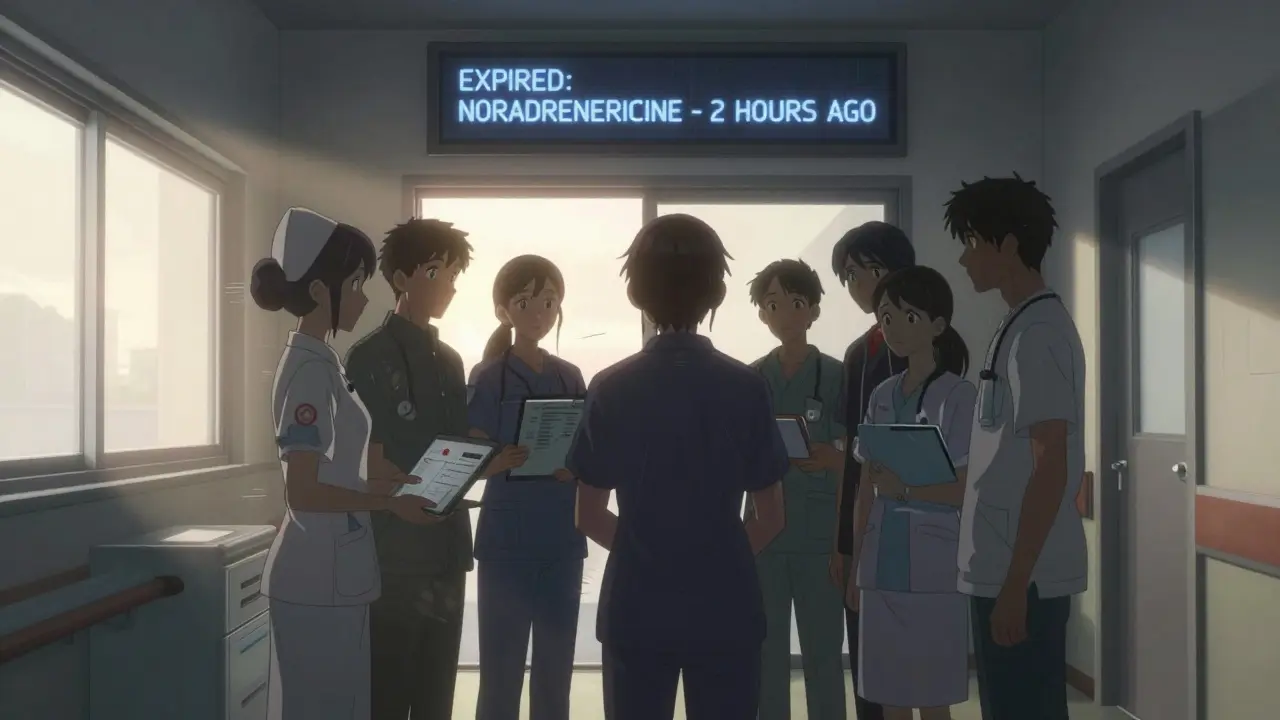
The Real Barrier: Lack of Pharmacists
The biggest reason hospitals struggle with expired meds isn’t money. It’s people. The American Association of Colleges of Pharmacy predicts a shortage of 112,000 pharmacists by 2027. Community hospitals already can’t afford full-time critical care pharmacists. So they rely on part-timers or none at all. That’s why 68.4% of community hospitals report inadequate medication management resources. And why the gap between academic centers (87% have protocols) and community hospitals (42%) keeps growing. If you’re in a small hospital, here’s what you can do:- Partner with a nearby academic center. Ask for their protocol. Most will share it.
- Use free ASHP resources. Their Drug Shortages Resource Center has downloadable checklists.
- Train your nurses. Teach them how to spot signs of withdrawal or overdose. They’re your eyes on the ground.
What’s Changing in 2026?
The ASHP is updating its guidelines this year. The new version will include specific protocols for expired medications-not just shortages. That’s huge. It means this won’t be an afterthought anymore. The FDA is also testing new expiration dating rules. Some drugs might now last longer than printed on the label. But until then, assume the date is final. And more hospitals are starting to tie reimbursement to medication safety. If your hospital has more than 15% of patients readmitted due to medication errors, CMS cuts your payments. That’s forcing change.Final Rule: Never Guess. Always Check.
There’s no shortcut. No magic pill. Just discipline. If a drug expires:- Don’t swap it with something that looks similar.
- Don’t use what’s left in the vial “just in case.”
- Don’t wait for the pharmacist to show up.
- Find your protocol.
- Know your tiers.
- Adjust the dose.
- Monitor like your patient’s life depends on it-because it does.

 Medications
Medications
Rachidi Toupé GAGNON
February 10, 2026 AT 17:25Bro this is the kind of post that makes me wanna hug a pharmacist 😭
Expired fentanyl? Nah, we got hydromorphone on deck like a boss. ASHP protocol? Printed, laminated, taped to the med cart.
One less nightmare in the ICU. You just saved someone’s life today, even if they don’t know it.