Most people don’t realize that a rough, dry patch on their cheek or scalp isn’t just an old sunburn or a harmless age spot. It could be an actinic keratosis - a precancerous lesion that, if left alone, might turn into skin cancer. These aren’t rare. In the U.S. alone, over 58 million people have them. And if you’ve spent years in the sun - whether you’re a gardener, a surfer, a construction worker, or just someone who loved the outdoors - you’re at risk.
What Exactly Is an Actinic Keratosis?
An actinic keratosis (AK), also called solar keratosis, is a patch of damaged skin caused by years of UV exposure. It doesn’t appear overnight. It builds up slowly, over decades. The skin cells in the top layer (epidermis) start to misbehave because of DNA damage from sunlight. At first, you might not even notice it. But when you run your fingers over your face, scalp, or hands, you’ll feel it: a rough, gritty spot that doesn’t smooth out like normal skin. That’s the classic sign - more often felt than seen. These patches can be red, pink, brown, gray, or even skin-colored. On darker skin tones, they often look like dark spots that don’t fade. They’re usually small - about the size of a pencil eraser - but can grow larger. Some develop a thick, horn-like bump on top, which is a red flag for higher cancer risk. They show up where the sun hits hardest: face, ears, scalp (especially if you’re bald), neck, forearms, and backs of hands. The big worry? About 10-15% of people with more than 10 AKs will develop squamous cell carcinoma (SCC), a type of skin cancer, within their lifetime. And here’s the key point: 90% of SCCs start as untreated AKs. That’s not a guess. It’s backed by decades of research. Treating AKs isn’t just about fixing a cosmetic issue - it’s stopping cancer before it starts.Why Field Treatments Are the Gold Standard
You can’t just treat one patch and call it done. That’s because the sun doesn’t just damage one spot - it damages a whole area. This is called "field cancerization." Your skin might look mostly normal, but underneath, hundreds of cells are already mutated. That’s why doctors now focus on field treatments - therapies that clear not just the visible lesions, but the invisible damage around them. There are three main types of field treatments:- Topical creams and gels - applied directly to the skin
- Chemical peels - using acids to remove damaged layers
- Photodynamic therapy (PDT) - using light-activated drugs
Topical Treatments: What Works and What to Expect
The most common topical treatments are 5-fluorouracil (5-FU), imiquimod, tirbanibulin, and ingenol mebutate. 5-Fluorouracil (5-FU) has been around since the 1970s. It’s cheap - generic versions cost about $120 for a full course. You apply it once or twice a day for 2 to 4 weeks. The downside? Your skin goes through hell. It gets red, swollen, crusty, and burns like fire. Many people stop early because it’s unbearable. But here’s the truth: if you stick with it, 75-85% of lesions clear. One patient on HealthUnlocked said, “Worth the 4 weeks of redness to stop cancer before it starts.” That’s the mindset. Imiquimod works differently. It doesn’t kill cells directly. Instead, it tricks your immune system into attacking the damaged skin. You apply it three times a week for up to 16 weeks. It’s less burning than 5-FU, but takes longer. Clearance rates are around 54-75%. It’s often used for thicker lesions on the scalp or lower legs. Tirbanibulin (brand name Klisyri) is the new kid on the block. Approved in 2020, it works in just 5 days. You apply it once a day for a week. It’s great for the face because it’s fast and has fewer side effects. But it costs about $650 per treatment. If you’re young, active, and want to get back to normal fast, it’s worth it. For older patients on a budget, 5-FU still wins. Ingenol mebutate is a two- or three-day treatment, but it’s been pulled from some markets due to safety concerns. It’s still used in Australia and parts of Europe, but not widely in the U.S.Chemical Peels and Photodynamic Therapy
Trichloroacetic acid (TCA) peels are another option. A dermatologist applies a chemical solution to the skin, which peels off the top layers. It’s done in-office, takes 15 minutes, and works well for large areas like the forehead or scalp. Recovery takes about a week. Side effects include redness and peeling - similar to a bad sunburn. Photodynamic therapy (PDT) is more advanced. First, a light-sensitive drug (aminolevulinic acid) is applied to the skin. After a few hours, you sit under a special blue or red light for 15-20 minutes. The light activates the drug, which destroys abnormal cells. You might need one or two sessions. Clearance rates are 44-75%. The big plus? It’s excellent for treating large areas with minimal scarring. The downside? You can’t go outside for 48 hours after treatment - your skin will burn in normal daylight.
How Do You Know It’s an AK and Not Something Else?
Not every rough patch is an AK. It could be eczema, psoriasis, or even a benign mole. Dermatologists use a simple rule: if it’s rough, persistent, and on sun-exposed skin, suspect AK. But there are warning signs that mean you need a biopsy:- It’s tender or painful
- It’s thicker than half a centimeter
- It bleeds or crusts without injury
- It grows quickly
- It has a raised, horn-like bump
Who’s at Risk - And Who Should Be Checked?
You’re at higher risk if you:- Have fair skin, light hair, or blue/green eyes
- Have a history of sunburns or tanning bed use
- Live in a sunny climate (Arizona, Florida, Australia)
- Are over 40
- Have a weakened immune system (from organ transplants, HIV, or certain medications)
What Happens If You Ignore It?
Some people think, “It’s just a rough patch. It’s not hurting me.” But here’s the reality: about 5-10% of individual AKs turn into squamous cell carcinoma over 10 years. For people with weakened immune systems, that number jumps to 25%. And once SCC develops, it can spread - especially if it’s ignored. The good news? If caught early, SCC is almost always curable with simple surgery. But if it grows deep or spreads to lymph nodes? Treatment becomes much harder. That’s why treating AKs is like wearing a seatbelt. You don’t do it because you expect to crash. You do it because you don’t want to find out what happens if you don’t.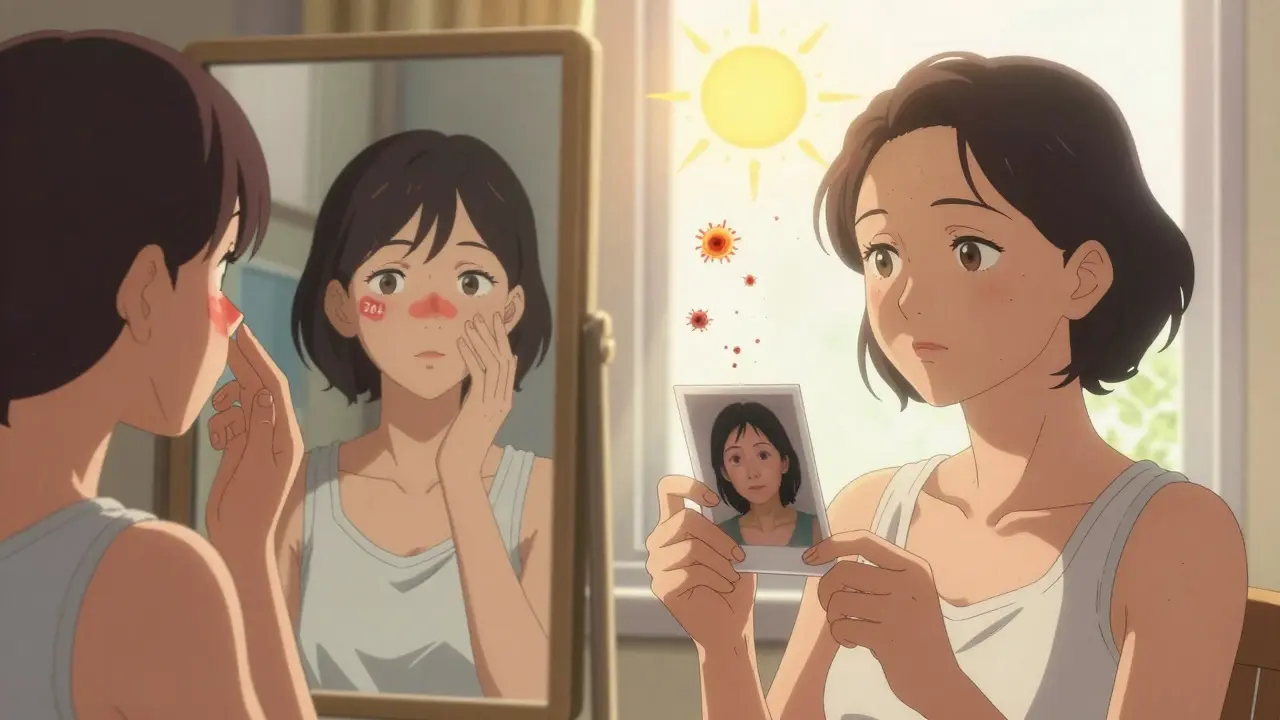
How to Prevent More AKs From Forming
Treatment clears what’s there. But prevention stops what’s next. The Skin Cancer Foundation found that patients who got proper sun protection counseling reduced new AKs by 37% over two years. That’s huge. Here’s what works:- Wear broad-spectrum SPF 30+ every day - even in winter
- Use a wide-brimmed hat and UV-blocking sunglasses
- Avoid direct sun between 10 a.m. and 4 p.m.
- Don’t use tanning beds - ever
- Check your skin monthly. Run your fingers over your face, ears, scalp, arms, and hands. If something feels rough, see a doctor.
What About Side Effects? Is It Worth the Pain?
Yes. But it’s not easy. Most field treatments cause inflammation. That’s how they work - your skin reacts, then heals clean. But 42% of patients on Amazon reviews say the burning and crusting were worse than they expected. Some quit treatment early. That’s a mistake. If you’re using 5-FU or imiquimod, expect:- Redness and swelling (day 3-7)
- Crusting and peeling (day 7-14)
- Itching or stinging
What’s Next? New Treatments on the Horizon
Research is moving fast. A 2023 study in JAMA Dermatology found that combining 5-FU with PDT cleared 92% of lesions - better than either alone. That’s promising. Scientists are also looking at treatments that target the skin’s microbiome. Some believe bad bacteria on sun-damaged skin help AKs grow. Others are testing drugs that block specific mutations in AK cells - like a precision strike on cancer before it starts. The bottom line? We’re getting smarter about preventing skin cancer. And the best tool we have right now is early treatment of actinic keratoses.Can actinic keratoses go away on their own?
Yes, but rarely - and it’s not safe to wait. About 10-20% of AKs may disappear without treatment, but they often come back. More importantly, even if one patch clears, the underlying sun damage remains. That means more lesions will likely form. Treating them stops the process before cancer develops.
Are actinic keratoses the same as skin cancer?
No - but they’re the earliest stage of it. AKs are precancerous. They haven’t invaded deeper layers of skin yet. But if left untreated, they can become squamous cell carcinoma, which is invasive and potentially dangerous. Doctors treat AKs like early cancer because 90% of SCCs start from them.
How long does it take for an AK to turn into skin cancer?
There’s no set timeline. For most people, it takes years - sometimes decades. But in high-risk groups (like transplant patients), it can happen in just 1-2 years. That’s why regular checks matter. Waiting for symptoms like pain or bleeding means it’s already advanced.
Can I treat AKs at home without seeing a doctor?
No. While some topical treatments are available by prescription, you need a doctor to confirm it’s an AK and not something more serious like melanoma. Self-diagnosis is risky. What looks like a dry patch could be early skin cancer. Always get a professional evaluation before starting treatment.
Do I need to keep checking my skin after treatment?
Yes - even after successful treatment. Sun damage is permanent. New AKs can form anywhere sun-exposed skin is damaged. Most doctors recommend annual skin exams. If you’ve had multiple AKs, you’re at higher risk for more. Monthly self-checks and yearly professional exams are the best defense.


 Medications
Medications
Robin Van Emous
January 26, 2026 AT 18:01Been dealing with these rough patches on my scalp for years-thought it was just dry skin. Turns out, it’s AKs. Got treated with 5-FU last year. Oof. Worst 4 weeks of my life. But? No more lesions. Worth every second of burning. Seriously.
rasna saha
January 27, 2026 AT 10:29Thank you for writing this. I’m from India, and we don’t talk enough about sun damage here. My dad had one on his ear-ignored it for two years. Now he’s getting regular checkups. This post could save lives.
Skye Kooyman
January 28, 2026 AT 10:07My dermatologist told me to use 5-FU. I said no. I’m still here. Still have the patch. Still not sure I’ll ever do it.