NMS Risk Assessment Tool
Neuroleptic Malignant Syndrome (NMS) is a potentially fatal medical emergency caused by the combination of certain medications. This tool helps you assess your risk of developing NMS when taking antipsychotics with metoclopramide.
Risk Factors
Combining metoclopramide with antipsychotic medications isn’t just a mild caution-it’s a potentially deadly mix. If you or someone you know is taking both, you need to understand the real risk: neuroleptic malignant syndrome (NMS). This isn’t a rare side effect you can ignore. It’s a medical emergency that can kill within hours if not caught early.
What Is Neuroleptic Malignant Syndrome?
NMS isn’t just another side effect. It’s a full-body crisis triggered when dopamine activity in the brain drops too low, too fast. The classic signs show up together: high fever (often above 102°F), stiff muscles that won’t relax, confusion or agitation, and wild swings in blood pressure, heart rate, or breathing. Your body starts to overheat from within, muscles break down, and your kidneys can fail. It happens in about 0.02% to 0.05% of people on antipsychotics alone-but when you add metoclopramide, the risk spikes.
Think of dopamine as the brain’s natural brake pedal for movement and temperature control. Antipsychotics slam that brake. Metoclopramide? It slams it harder. Together, they don’t just slow you down-they lock the wheels.
Why Metoclopramide Is a Hidden Risk
Most people think of metoclopramide as a simple nausea pill. It’s sold as Reglan or Gimoti, used for heartburn, gastroparesis, or chemo-induced vomiting. But it’s not harmless. Metoclopramide blocks dopamine receptors in the brain-just like haloperidol, risperidone, olanzapine, and other antipsychotics. It’s not a coincidence that the FDA label for Reglan says: Avoid Reglan in patients receiving other drugs associated with NMS, including typical and atypical antipsychotics.
This isn’t a theoretical warning. There are documented cases where people on antipsychotics for schizophrenia or bipolar disorder developed NMS after being given metoclopramide for vomiting. One patient, 68, on risperidone for years, got metoclopramide for nausea after surgery. Within 36 hours: fever of 104°F, rigid limbs, confusion, and creatine kinase levels 10 times normal. He survived-only because his doctor recognized NMS fast.
The Double Hit: Pharmacodynamics and Pharmacokinetics
The danger isn’t just that both drugs block dopamine. It’s worse than that.
First, there’s the pharmacodynamic hit: both drugs do the same thing-block dopamine receptors. Add them together, and the effect isn’t 1+1=2. It’s 1+1=5. Your brain gets flooded with dopamine blockade, triggering NMS.
Then there’s the pharmacokinetic hit: many antipsychotics, like haloperidol and risperidone, block the liver enzyme CYP2D6. That’s the same enzyme that breaks down metoclopramide. So when you take them together, metoclopramide doesn’t get cleared. It builds up. Your blood levels can double or triple. You’re not just getting two drugs that fight dopamine-you’re getting a much higher dose of one of them.
This is especially dangerous for older adults, people with kidney problems, or those with a genetic variation that slows CYP2D6. Up to 7% of people of European descent have this slow-metabolizer profile. They’re walking into a storm with no umbrella.
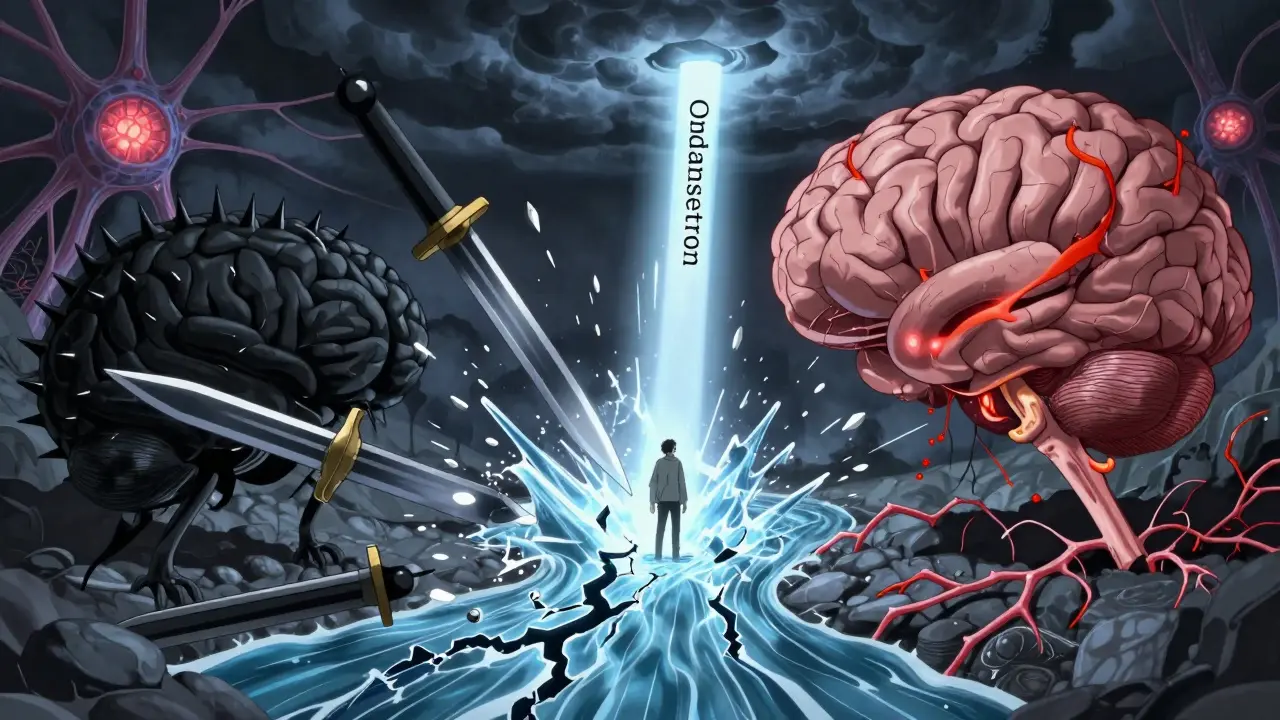
What’s Safer Than Metoclopramide?
If you’re on an antipsychotic and need something for nausea or stomach motility, metoclopramide is not the answer. There are safer options that don’t touch dopamine at all.
- Ondansetron (Zofran) blocks serotonin receptors. It’s the go-to for chemo nausea and works great without touching dopamine.
- Promethazine (Phenergan) blocks histamine and acetylcholine. It’s not perfect-it can cause drowsiness and low blood pressure-but it doesn’t cause NMS.
- Dexamethasone is a steroid sometimes used for nausea in cancer patients. No dopamine interaction.
- Prokinetic alternatives like erythromycin (an antibiotic with prokinetic effects) can help with gastroparesis without dopamine blockade.
Doctors should be asking: Is this patient on an antipsychotic? Then don’t reach for metoclopramide. The alternatives exist. They’re proven. They’re safer.
Who’s Most at Risk?
This isn’t a risk for everyone. But certain people are sitting on a ticking clock:
- Anyone on typical antipsychotics like haloperidol or fluphenazine-these are stronger dopamine blockers than newer ones.
- People with Parkinson’s disease or a history of movement disorders-metoclopramide is outright contraindicated here.
- Patients with renal impairment-metoclopramide builds up in the blood if kidneys can’t clear it.
- Those on CYP2D6 inhibitors like fluoxetine, paroxetine, or bupropion-these antidepressants also slow metoclopramide breakdown.
- Anyone who’s had tardive dyskinesia before-metoclopramide can make it worse or trigger it again.
And here’s the kicker: metoclopramide carries a Boxed Warning from the FDA for tardive dyskinesia-the same warning given to antipsychotics. That’s how serious this is. The longer you take it, the higher the risk. The FDA says: don’t use it for more than 12 weeks. Period.
What to Do If You’re Already Taking Both
If you’re on metoclopramide and an antipsychotic right now, don’t panic. But don’t wait either.
Step 1: Make a full list of every medication you take-prescription, over-the-counter, supplements. Include doses and how long you’ve been on each.
Step 2: Bring it to your doctor or pharmacist. Say: “I’m on [antipsychotic name] and metoclopramide. I’ve heard this combination can cause NMS. Is this safe?”
Step 3: If you develop any of these symptoms-fever, stiff muscles, confusion, fast heartbeat, dark urine-go to the ER immediately. Don’t wait. NMS can kill in 24 to 72 hours if untreated.
Step 4: If you’ve been on metoclopramide for more than 12 weeks, ask about stopping it-even if you feel fine. Tardive dyskinesia can appear months after stopping, and it’s often permanent.
Why This Interaction Is Still Happening
You’d think this warning would be enough. But it’s not. Why?
Many doctors still see metoclopramide as a “safe” nausea drug. It’s cheap. It’s been around since 1980. It’s in the formulary. Pharmacists don’t always flag it. Patients don’t know to ask.
And when a patient with schizophrenia gets nauseous after eating, the easiest fix is metoclopramide. The right fix? Ondansetron. But if the prescriber doesn’t know the risk-or hasn’t been reminded by a pharmacist-they keep reaching for the old standard.
It’s not malpractice. It’s ignorance. And it’s costing lives.
The Bottom Line
Metoclopramide and antipsychotics don’t just interact-they collide. The result isn’t a side effect. It’s a life-threatening emergency. The FDA, NCBI, and top pharmacy schools all agree: avoid this combination.
If you’re on an antipsychotic, don’t take metoclopramide. Period.
If you’re a clinician, don’t prescribe it. There are safer alternatives. Use them.
If you’ve been on both for weeks or months, talk to your doctor now. Don’t wait for a fever. Don’t wait for stiff limbs. NMS doesn’t warn you. It strikes.
Your body doesn’t need two dopamine blockers. It needs one less.
Can metoclopramide cause neuroleptic malignant syndrome on its own?
Yes, though it’s rare. Metoclopramide alone can trigger NMS, especially at high doses or in people with kidney problems. But the risk skyrockets when combined with antipsychotics. The FDA warns against using it with any drug linked to NMS-not just antipsychotics, but also drugs like haloperidol, risperidone, and even some anti-nausea meds with dopamine-blocking effects.
How long does it take for NMS to develop after taking both drugs?
NMS can appear within hours or take up to several days. Most cases start within 1 to 3 days after starting or increasing the dose of either drug. But there are reports of symptoms appearing after just one dose, especially in people already on antipsychotics. Don’t assume it’s safe just because you’ve been on metoclopramide for weeks-adding an antipsychotic can trigger it suddenly.
Is there a blood test to confirm NMS?
There’s no single test that diagnoses NMS. But doctors check for high creatine kinase (CK) levels-often 5 to 10 times normal-which means muscles are breaking down. Elevated liver enzymes, high white blood cell count, and abnormal electrolytes (like low calcium or high phosphate) are also common. Temperature and mental status changes are clinical signs, not lab results. Diagnosis is based on symptoms + lab findings + recent drug exposure.
Can I take metoclopramide if I’m on an atypical antipsychotic like olanzapine?
No. Atypical antipsychotics like olanzapine, quetiapine, and aripiprazole still block dopamine receptors-just less strongly than older ones. But they still carry the same NMS risk when combined with metoclopramide. The FDA warning includes both typical and atypical antipsychotics. The mechanism is the same. The danger is real. Don’t assume newer means safer in this case.
What should I do if my doctor prescribes metoclopramide while I’m on an antipsychotic?
Ask for a second opinion or ask your pharmacist to review the interaction. Say: “I’m on [antipsychotic name]. The FDA says not to combine it with metoclopramide because of NMS risk. Is there a safer alternative?” Ondansetron, promethazine, or dexamethasone are common substitutes. If your doctor insists, ask them to document the risk and your informed consent in writing. Your life is worth more than convenience.


 Medications
Medications