Most people think hemorrhoids are just an embarrassing itch or a painful lump. But they’re more than that-they’re swollen veins in your rectum or anus, and they happen to 75% of people at some point in their lives. The real problem? Many don’t know if what they’re feeling is internal or external, or what to do about it. And that confusion leads to delays, wrong treatments, and unnecessary suffering.
What’s the Difference Between Internal and External Hemorrhoids?
It all comes down to location-and whether or not you feel pain.
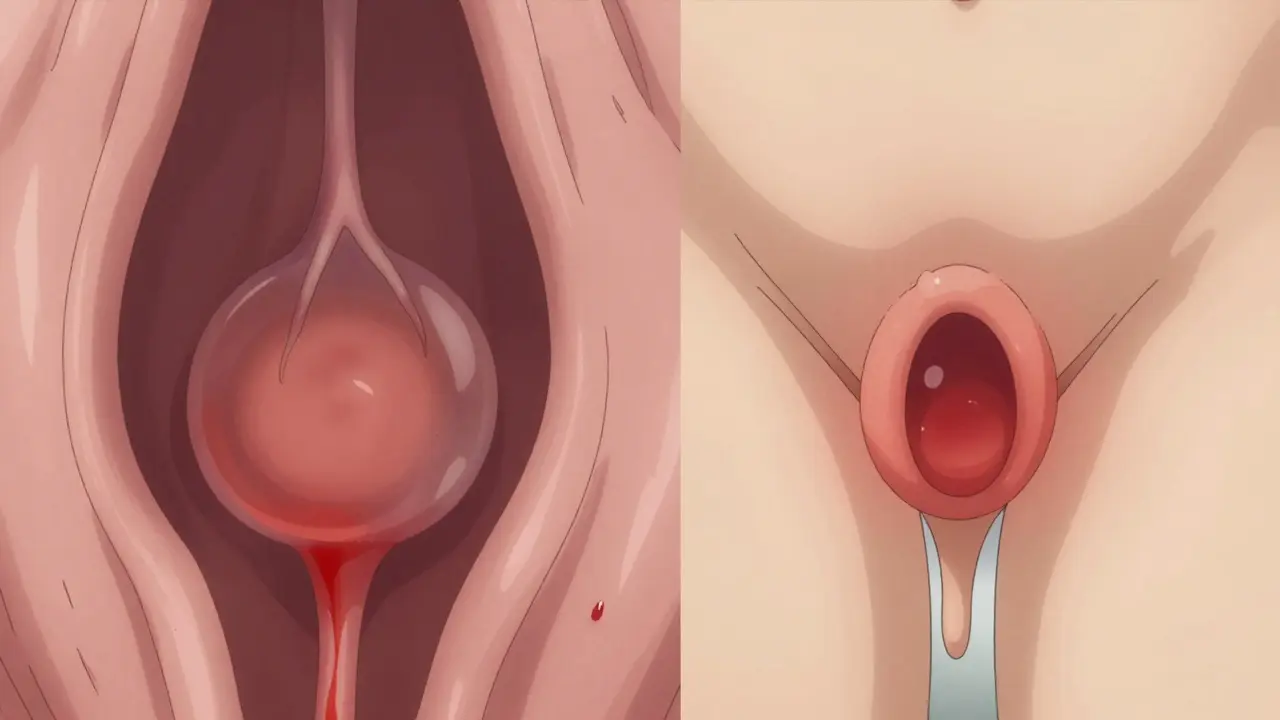
Internal hemorrhoids sit inside the rectum, above a line called the dentate line. This area has no pain receptors, so even when they swell, you might not feel a thing. The main sign? Bright red blood on your toilet paper, in the bowl, or on your stool. It’s usually painless, which is why many people ignore it-until it gets worse. Internal hemorrhoids can also prolapse, meaning they push out through the anus. When that happens, you might feel a soft lump, pressure, or the sensation that you haven’t fully emptied your bowels.
External hemorrhoids form under the skin around the anus. This area is packed with nerves. So when these veins swell, you feel it. Think: sharp pain, burning, itching, or a noticeable lump you can touch. The worst kind? Thrombosed external hemorrhoids. That’s when a blood clot forms inside the vein. It turns into a hard, purple or blue lump that feels like a marble under your skin. Sitting becomes torture. Standing hurts. Walking? Forget it.
And here’s something most don’t realize: you can have both at the same time. One person might have a bleeding internal hemorrhoid and a painful external one. That’s why symptoms can feel confusing. Is it bleeding? Is it pain? Is it both? The answer is often yes.
Why Do Hemorrhoids Happen?
They’re not caused by sitting too long on the toilet (though that doesn’t help). They happen because of pressure-constant, repeated pressure on the veins in your lower rectum.
Common triggers:
- Chronic constipation and straining during bowel movements
- Diarrhea that lasts too long
- Pregnancy-up to 35% of pregnant women get them, especially in the third trimester
- Obesity
- Lifting heavy weights regularly
- Sitting for hours, especially on the toilet
Here’s a fact most people miss: your toilet position matters. If your knees are lower than your hips, you’re straining more. A simple footstool under your feet-like a small stool or even a stack of books-lifts your knees above your hips. That reduces pressure on your rectal veins by about 30%. It’s not magic. It’s physics.
When Is It Not a Hemorrhoid?
Rectal bleeding is scary. And most people assume it’s hemorrhoids. But it’s not always.
Anal fissures-small tears in the lining of the anus-also cause bleeding. But they come with a sharp, tearing pain during bowel movements, not the dull ache or itching of hemorrhoids. Fissures rarely cause lumps. They cause a visible crack. And they don’t respond to hemorrhoid creams.
Even more serious: colorectal cancer, inflammatory bowel disease (like Crohn’s or ulcerative colitis), or polyps can cause bleeding too. That’s why if you’re over 50, have a family history of colon cancer, or notice changes in bowel habits-like narrower stools, unexplained weight loss, or persistent fatigue-you need to see a doctor. Don’t self-diagnose. Bleeding isn’t just a hemorrhoid problem.

What Treatments Actually Work?
For mild cases, you don’t need surgery. You need lifestyle changes.
Step 1: Fiber and water
Eat 25-30 grams of fiber daily. That’s two cups of cooked lentils, or a bowl of oatmeal with berries and chia seeds, plus a whole apple. Most people get less than half that. Add 8-10 glasses of water. Fiber pulls water into your stool so it moves smoothly. No straining. No pressure. No flare-ups.
Step 2: Sitz baths
Fill a tub with warm (not hot) water, just enough to cover your bottom. Sit for 15-20 minutes, 2-3 times a day. It reduces swelling and soothes irritation. No fancy gadgets. Just warm water and patience.
Step 3: Over-the-counter help
Hydrocortisone cream (1%) can ease itching and swelling. Witch hazel pads (like Tucks) reduce inflammation. Avoid products with benzocaine or lidocaine long-term-they numb the pain but don’t fix the cause, and can irritate skin over time.
What About Procedures?
If home care doesn’t help after a week or two, or if you’re bleeding a lot, it’s time for medical help.
For internal hemorrhoids:
- Rubber band ligation: A tiny rubber band is placed around the base of the hemorrhoid. It cuts off blood flow. The hemorrhoid shrinks and falls off in 5-7 days. It’s 90% effective for Grades I-III. You might feel pressure or mild cramping for a day or two.
- Sclerotherapy: A chemical is injected into the hemorrhoid to shrink it. Less painful than banding, but slightly less effective.
- Infrared coagulation: A small probe uses heat to scar the tissue. Good for small hemorrhoids.
For thrombosed external hemorrhoids:
If you have a sudden, painful, purple lump, see a doctor within 72 hours. They can make a tiny cut and remove the clot. The pain drops almost immediately. Waiting longer means more swelling, more healing time, and more discomfort.
Surgery for severe cases:
If hemorrhoids keep coming back, or they’re Grade IV (always prolapsed), surgery might be needed.
- Hemorrhoidectomy: The hemorrhoid is cut out. It’s the most effective option-95% success rate. But recovery takes 2-4 weeks. Pain is real. You’ll need painkillers.
- Stapled hemorrhoidopexy: Instead of removing the hemorrhoid, they reposition it and cut off blood flow. Less pain than a full removal, but higher chance of recurrence.
What Doesn’t Work (and Why You Should Avoid It)
Online ads promise miracle cures: herbal ointments, essential oil suppositories, “natural” hemorrhoid pills. None of these are backed by science. The American Gastroenterological Association warns against them. Some contain steroids or unregulated ingredients that can damage skin or mask symptoms.
And don’t rely on “just wait it out.” Hemorrhoids don’t disappear on their own. They get worse. And delaying treatment increases your chance of complications-like chronic pain, infection, or anemia from ongoing bleeding.

How to Prevent Them From Coming Back
Treatment fixes the problem. Prevention stops it from returning.
- Keep fiber high. Stick to 30g daily. Use a food tracker if you need to.
- Drink water. Aim for clear or light yellow urine.
- Don’t sit on the toilet longer than 5 minutes. No phones. No books. Just go.
- Move. Walk 30 minutes a day. Even if it’s just around the house.
- For pregnant women: sleep on your left side. It takes pressure off your pelvic veins.
Studies show people who stick to these habits have a 5-10% chance of recurrence. Those who don’t? Up to 50%.
When to See a Doctor
You don’t need to wait until it’s unbearable. Call your GP if:
- Bleeding lasts more than a week
- Pain doesn’t improve after a week of home care
- You feel dizzy, weak, or fatigued (signs of blood loss)
- Your stool is dark, tarry, or black (could mean bleeding higher up)
- You notice changes in bowel habits or unexplained weight loss
It’s not weakness to ask for help. It’s smart.
Can internal hemorrhoids turn into external ones?
No, they don’t turn into each other. They’re different types based on location. But an internal hemorrhoid can prolapse and bulge outside the anus, which might look like an external one. That’s still an internal hemorrhoid that’s protruding-not a new type.
Are hemorrhoids dangerous?
Usually not. But they can lead to complications. Severe bleeding can cause anemia. Thrombosed external hemorrhoids can become infected. And if you ignore bleeding, you might miss something more serious like cancer. That’s why diagnosis matters.
Can I use ice packs for external hemorrhoids?
Yes, but only short-term. Wrap ice in a cloth and apply for 10 minutes at a time to reduce swelling and numb pain. Don’t use it directly on skin or for longer than 15 minutes. Ice doesn’t treat the cause, but it can give you relief while you start other treatments.
Do hemorrhoids go away on their own?
Small ones might shrink with better habits, but they rarely disappear completely. Without changes to diet, bowel habits, or posture, they’ll likely come back. Think of them like a flare-up of chronic inflammation-it needs ongoing management.
Is it safe to pop a thrombosed hemorrhoid at home?
Absolutely not. Trying to pop it yourself can cause infection, severe bleeding, or scarring. Only a doctor should drain a thrombosed hemorrhoid, and only within the first 72 hours for best results.
Final Thought
Hemorrhoids are common. They’re not shameful. But they’re not something to ignore. Whether it’s a tiny bleed or a painful lump, the right steps-fiber, water, posture, and knowing when to see a doctor-can turn a frustrating problem into a manageable one. You don’t need a miracle cure. You need clarity. And action.

 Medications
Medications
steve ker
January 13, 2026 AT 10:02Stop overcomplicating it.
Rebekah Cobbson
January 14, 2026 AT 01:36People need to know it’s not shameful to ask for help.
Audu ikhlas
January 14, 2026 AT 14:08Stop treating this like a medical crisis its just your body telling you to stop being lazy
Sonal Guha
January 15, 2026 AT 13:58Don't mistake anecdotal relief for clinical efficacy.
TiM Vince
January 16, 2026 AT 14:36Also their fiber intake is insane. Miso soup, seaweed, beans. No wonder.
gary ysturiz
January 18, 2026 AT 12:25Progress not perfection. You're already ahead of most people just by reading this.
Jay Powers
January 19, 2026 AT 22:51Doctors aren't judging you. They've seen it all.
Lawrence Jung
January 20, 2026 AT 16:33The real treatment is a return to simplicity. No creams. No gadgets. Just movement. Just food. Just breath.
Modern medicine has turned a natural process into a product market
Alice Elanora Shepherd
January 21, 2026 AT 16:48Also - please, for the love of all that is holy - don’t use benzocaine long-term. It’s a trap.
Lauren Warner
January 23, 2026 AT 15:38And your fiber advice? Useless without context. Soluble vs insoluble? Fermentable carbs? You’re giving people a recipe for bloating and gas.
Craig Wright
January 24, 2026 AT 06:45And yes - your posture advice is correct. But no one will listen until the government mandates ergonomic toilets.
Rinky Tandon
January 24, 2026 AT 11:30Western medicine is terrified of natural solutions because they can’t patent them.
Ben Kono
January 25, 2026 AT 14:08