By the time most people hear the words type 2 diabetes, the damage has already been building for years. It doesn’t come out of nowhere. It starts quietly-with fatigue, weight that won’t budge, cravings that won’t quit, and a waistline that keeps growing. Behind those symptoms is a silent breakdown: your body’s cells are no longer listening to insulin. That’s insulin resistance. And it’s the engine driving not just diabetes, but a whole cluster of health problems known as metabolic syndrome.
What Exactly Is Insulin Resistance?
Insulin is your body’s key to unlocking cells so glucose-your main source of energy-can get inside. When you eat, your pancreas releases insulin to tell muscle, fat, and liver cells: Take in the sugar. But with insulin resistance, those cells start ignoring the signal. Glucose stays in your blood. Your pancreas responds by pumping out more insulin to compensate. That’s called hyperinsulinemia. This isn’t just a glitch. It’s a full-blown cellular malfunction. High levels of sugar and fat in the blood, especially from constant snacking and processed carbs, overload the insulin signaling pathway. The message gets blocked. Inflammation kicks in. Fat builds up in the liver and muscles. The endoplasmic reticulum, which helps proteins fold properly, gets stressed. Oxidative damage piles up. All of this makes insulin less effective. Here’s the scary part: 80 to 90% of people with type 2 diabetes have insulin resistance before they’re even diagnosed. Dr. Ralph DeFronzo’s research from the University of Texas Health Science Center showed this decades ago-and it still holds true today. Insulin resistance isn’t a side effect of diabetes. It’s the main reason diabetes develops.Metabolic Syndrome: More Than Just a Label
Metabolic syndrome isn’t a disease. It’s a warning sign. It’s when five risk factors show up together: excess belly fat, high triglycerides, low HDL (good) cholesterol, high blood pressure, and elevated fasting blood sugar. You need at least three of these to be diagnosed. The International Diabetes Federation updated the criteria in 2023. For men in Europe, a waist size of 94 cm or more counts. For South Asian, Chinese, or Japanese men, it’s 90 cm. For women, it’s 80 cm across most ethnic groups. These aren’t arbitrary numbers. They reflect where fat is stored-and where it does the most harm. That belly fat? It’s not just cosmetic. Visceral fat around your organs releases inflammatory chemicals and free fatty acids that directly interfere with insulin. That’s why two people can weigh the same, but only one has metabolic syndrome. Genetics, diet, and activity levels determine where fat goes. And where it goes, determines your risk. In 2024, experts started pushing to rename metabolic syndrome to metabolic dysfunction syndrome (MDS). The old name made it sound like a list of symptoms. The new one says: this is broken biology. It’s not just high numbers. It’s your metabolism failing.How Insulin Resistance Turns Into Diabetes
Your pancreas can keep up for a while. It pumps out more insulin to force glucose into stubborn cells. But beta cells aren’t invincible. Over time, they burn out. Dr. Steven Kahn’s research at Joslin Diabetes Center found beta cell function declines about 4 to 5% per year in people heading toward type 2 diabetes. When insulin production drops below what’s needed to control blood sugar, glucose levels rise past the danger line: fasting glucose above 126 mg/dL (7.0 mmol/L) or post-meal glucose over 200 mg/dL (11.1 mmol/L). That’s when you cross from prediabetes into full-blown diabetes. Prediabetes isn’t a diagnosis you can ignore. It’s your last chance to turn things around. The Diabetes Prevention Program showed that people with metabolic syndrome and prediabetes had a 5 to 6 times higher risk of developing type 2 diabetes than those without. But here’s the good news: lifestyle changes cut that risk by 58% over three years.
Why This Matters Beyond Blood Sugar
Metabolic syndrome doesn’t just lead to diabetes. It leads to heart attacks, strokes, and kidney disease. The Mayo Clinic found that having metabolic syndrome increases your risk of heart disease by 200 to 300%. That’s because the same forces-insulin resistance, inflammation, fat buildup, and high blood pressure-damage blood vessels and promote plaque. Nonalcoholic fatty liver disease (NAFLD) is another silent partner. Up to 70% of people with metabolic syndrome have fat in their liver. If it progresses to NASH (inflammation and scarring), your risk of diabetes more than doubles. And it’s not just the liver. Fat builds up in the heart, kidneys, and even the pancreas itself, making the problem worse. Some experts, like Dr. Anna Gloyn from Oxford, argue that in certain groups-especially lean South Asians-beta cell failure might come first. Genetics can make the pancreas more fragile. But even then, insulin resistance still plays a major role. The American Association of Clinical Endocrinologists says insulin resistance is the unifying thread tying together obesity, diabetes, fatty liver, and heart disease.What You Can Actually Do About It
The good news? Insulin resistance is reversible-at least in its early stages. You don’t need magic pills or extreme diets. You need consistent, doable changes.- Weight loss: Losing just 5 to 7% of your body weight improves insulin sensitivity dramatically. For someone weighing 200 pounds, that’s 10 to 14 pounds. The Look AHEAD trial showed that people who lost 10% of their weight in a year had a 51% chance of reversing prediabetes.
- Exercise: Aim for 150 minutes a week of brisk walking, cycling, or swimming. Strength training twice a week helps too-muscle is the body’s biggest glucose sink.
- Diet: Cut back on sugary drinks, white bread, pastries, and processed snacks. Focus on vegetables, lean proteins, whole grains, nuts, and healthy fats. Fiber slows sugar absorption. Protein and fat help you stay full longer.
- Medication: Metformin is the first-line drug for prediabetes with metabolic syndrome. It lowers liver glucose production and improves insulin sensitivity. In the Diabetes Prevention Program, it reduced diabetes risk by 31% over three years.
Monitoring Progress: What to Track
Don’t wait for symptoms to get worse. Track your numbers.- HbA1c: This measures average blood sugar over 3 months. Normal is under 5.7%. Prediabetes is 5.7-6.4%. Diabetes is 6.5% or higher. Aim for under 7% if you have diabetes.
- Waist circumference: Measure at the narrowest point between ribs and hips. Track changes every 3 months.
- Fasting glucose: Check every 6-12 months if you’re prediabetic.
- Triglycerides and HDL: These lipids tell you about fat metabolism. High triglycerides and low HDL are red flags.
What’s Next? Hope on the Horizon
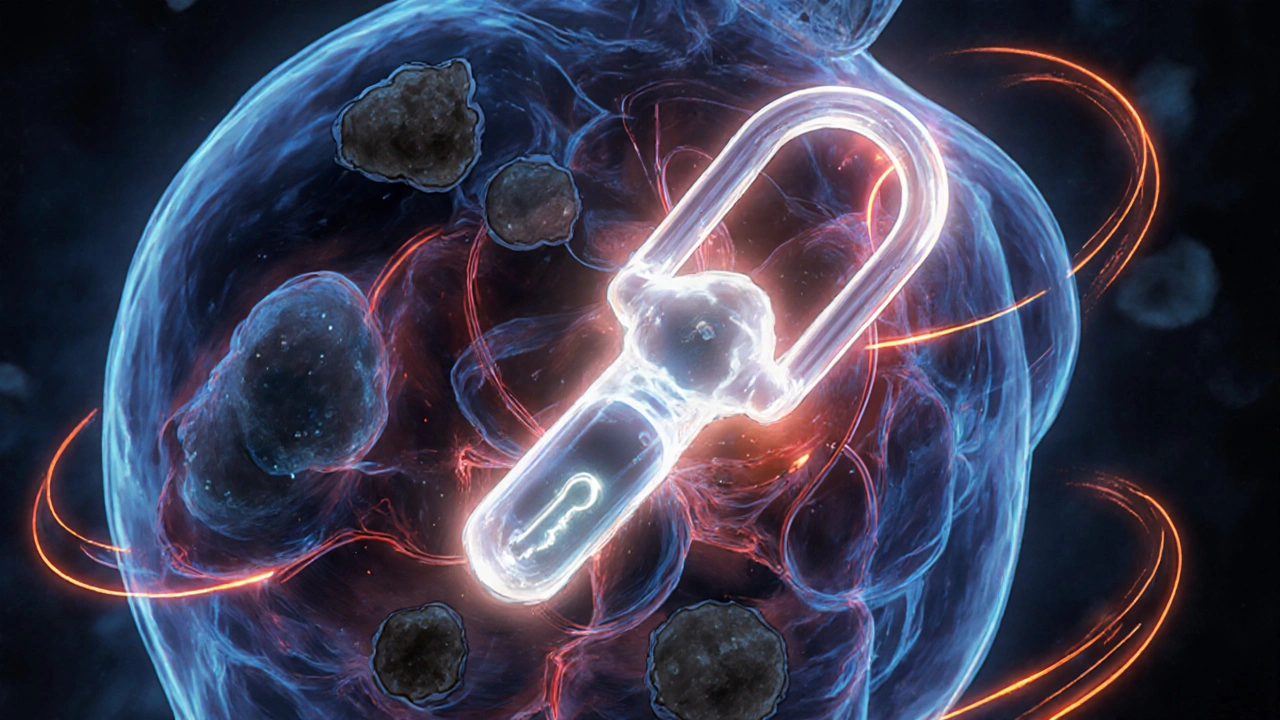
Research is moving fast. The NIH is investing $1.2 billion into beta cell preservation. Vertex Pharmaceuticals’ stem cell therapy, VX-880, helped 71% of patients reach HbA1c under 7% without insulin in Phase 3 trials. That’s not science fiction-it’s happening now. The European Association for the Study of Diabetes plans to update diagnostic criteria for metabolic dysfunction syndrome by late 2025. This isn’t just about labels. It’s about catching the problem earlier, treating it more aggressively, and preventing complications before they start. The World Health Organization warns that without action, diabetes-related deaths could rise 76% by 2045. But the Lancet Commission on Obesity says coordinated efforts-better food policies, access to care, community support-could cut type 2 diabetes incidence by 40 to 60% by 2035.Final Thought: This Is Your Body Asking for Help
Insulin resistance and metabolic syndrome aren’t punishments. They’re signals. Your body is telling you it’s overwhelmed. The good news? You’re not helpless. You’re not doomed. You’re just at a turning point. You don’t need to be perfect. You just need to be consistent. One less sugary drink. One extra walk. One better meal. Over time, those small choices rebuild your metabolism. They restore your body’s ability to respond to insulin. They turn a diagnosis into a second chance. The clock is ticking-but it’s not running out. It’s just counting down to the moment you decide to act.Can you reverse insulin resistance?
Yes, especially in the early stages. Losing 5-7% of body weight, exercising 150 minutes a week, and eating a whole-foods diet can significantly improve insulin sensitivity. Studies like the Diabetes Prevention Program and Look AHEAD show many people reverse prediabetes entirely within a year. Medications like metformin help, but lifestyle changes are the most powerful tool.
Is metabolic syndrome the same as type 2 diabetes?
No. Metabolic syndrome is a cluster of risk factors-like high blood pressure, belly fat, and elevated blood sugar-that increase your chance of developing type 2 diabetes and heart disease. Not everyone with metabolic syndrome has diabetes, but most people with type 2 diabetes have metabolic syndrome. It’s a warning sign, not the final diagnosis.
Why do some thin people get type 2 diabetes?
While obesity is the biggest risk factor, genetics matter. Some people, especially those of South Asian descent, store fat deep inside the abdomen and liver-even if they look lean. This visceral fat causes insulin resistance. Beta cell dysfunction can also play a stronger role in these cases. About 10-15% of people with type 2 diabetes are not overweight.
Do I need medication if I have metabolic syndrome?
Not always. Many people improve with diet, exercise, and weight loss alone. But if your blood sugar is already in the prediabetes range (HbA1c 5.7-6.4%) and you have other risk factors, your doctor may recommend metformin. It’s proven to reduce diabetes risk by 31%. Medication is a tool-not a failure. It gives your body time to heal while you make lifestyle changes.
How long does it take to see improvements in insulin sensitivity?
You can see changes in as little as 2-4 weeks. Blood sugar levels drop after reducing sugar and increasing activity. HbA1c, which reflects 3 months of average levels, takes longer. Most people see noticeable improvement in fasting glucose and triglycerides within 3 months of consistent lifestyle changes. Weight loss and fitness improvements follow over 6-12 months.
Can metabolic syndrome lead to other health problems?
Absolutely. It’s strongly linked to heart disease, stroke, nonalcoholic fatty liver disease (NAFLD), kidney disease, sleep apnea, and even certain cancers. The same inflammation and insulin resistance that drive diabetes also damage blood vessels and organs. Treating metabolic syndrome isn’t just about avoiding diabetes-it’s about protecting your whole body.
Are there any new treatments on the horizon?
Yes. GLP-1 and GIP receptor agonists like semaglutide and tirzepatide are revolutionizing treatment-they help with weight loss, blood sugar control, and heart protection. Stem cell therapies are being tested to replace damaged beta cells. Continuous glucose monitors are becoming more accurate and affordable. Research into gut microbiome and inflammation is also opening new pathways for prevention and reversal.

 Medications
Medications
Scott Walker
November 13, 2025 AT 23:14Man, this post hit different. I’ve been chasing my own insulin resistance for years, and honestly? The part about belly fat being the real villain made me pause. I thought it was just about calories, but nope - it’s where the fat hides. Thanks for the clarity. 🙏
Sharon Campbell
November 15, 2025 AT 03:52idk why ppl make this so complicated. just eat less sugar and move. done.
Ashley B
November 15, 2025 AT 15:18Let me guess - Big Pharma pushed this whole 'insulin resistance' narrative to sell metformin and Ozempic. They’ve been lying to us since the 70s about fat being the enemy. It’s all about insulin spikes and processed seed oils. The government and ADA are in bed with the food industry. You think your 'lifestyle changes' are helping? Nah. You’re just being manipulated into buying more junk food labeled 'low-fat' that’s full of corn syrup. Wake up.
And don’t even get me started on CGMs. They’re not for health - they’re surveillance tools for insurance companies to raise your premiums. I’ve seen the documents. They track your every bite. Your glucose readings are being sold to advertisers. You think you’re in control? You’re a data point.
And why is everyone so obsessed with weight loss? What if your body is just fine? What if insulin resistance is your body’s way of protecting you from toxins? What if the real problem is glyphosate in your food and PFAS in your water? No one talks about that. Because it’s not profitable.
They want you to believe you’re broken. But you’re not. You’re being poisoned. And the solution isn’t more pills or more exercise - it’s a complete systemic overhaul. Organic food. No plastic. No processed crap. And if you’re still sick after that? Then maybe it’s not your fault. Maybe it’s the world they built for you.
And yes, I’ve read the studies. All of them. And they’re funded by the same companies that profit from your disease. You think Dr. Kahn is neutral? He’s got grants from Novo Nordisk. Wake up.
sara styles
November 15, 2025 AT 22:00Everyone’s talking about metformin like it’s some miracle drug, but have you even looked at the long-term side effects? B12 deficiency? Gut microbiome destruction? Lactic acidosis? And don’t even get me started on the fact that metformin was originally derived from French lilac - a plant used in medieval times to treat plague symptoms. So we’re basically treating metabolic syndrome with a medieval antiseptic? That’s not science - that’s alchemy with a FDA stamp.
And the whole '5-7% weight loss' thing? That’s a placebo number. You think losing 10 pounds magically fixes your cellular insulin receptors? No. It just makes your clothes fit better. The real problem is mitochondrial dysfunction caused by chronic inflammation from ultra-processed foods - not your waistline. The FDA doesn’t even test for mitochondrial health in their diabetes guidelines. Why? Because they can’t patent mitochondria.
And why is everyone ignoring the circadian rhythm angle? Eating late at night spikes insulin when your body should be in repair mode. But no one talks about that because it doesn’t sell supplements. The real solution? Eat within an 8-hour window. Stop snacking. Let your pancreas rest. But of course, the food industry wants you grazing all day. That’s why they sell 'snack packs' and 'on-the-go' meals. It’s not about hunger - it’s about profit.
And don’t even mention intermittent fasting unless you’ve read Dr. Jason Fung’s 12-volume treatise on insulin and fasting. You think your 'walk after dinner' is enough? That’s like putting a Band-Aid on a severed artery. You need to rewire your entire metabolic programming. And no, Ozempic isn’t the answer - it’s a chemical crutch. You’re just delaying the inevitable crash when you stop taking it.
And why is no one asking why South Asians get diabetes at lower BMIs? Because their ancestral genes evolved to store fat in the liver during famines. Now they’re eating Twinkies. Their bodies are still in famine mode. But the CDC doesn’t have a 'genetic famine adaptation' category. They just say 'you’re obese.' That’s racism disguised as science.
And what about the role of sleep apnea? You think your high triglycerides are from sugar? No - they’re from oxygen deprivation at night. Your liver goes into stress mode and starts dumping glucose. But no one checks your AHI score before prescribing metformin. Because sleep studies cost money. And Big Pharma doesn’t want you sleeping better - they want you medicated.
And don’t even get me started on the gut microbiome. You think probiotics are just yogurt? No. Your gut bacteria produce short-chain fatty acids that regulate insulin signaling. But glyphosate kills them. And glyphosate is in 90% of conventional grains. So you’re eating a pesticide-laced loaf of 'whole wheat' bread and wondering why you’re insulin resistant. The answer isn’t exercise - it’s organic rye.
And who funded the Look AHEAD trial? The NIH? The CDC? No - it was the American Diabetes Association, which takes millions from food corporations. You think they want you to reverse diabetes? They want you to stay diabetic so you keep buying their products. This isn’t medicine - it’s a business model.
So yes - lose weight. Walk. Eat veggies. But don’t fool yourself. You’re still trapped in a system designed to keep you sick. The only real cure? Get off the grid. Move to the woods. Grow your own food. Stop trusting anyone with a white coat and a corporate logo.
Brendan Peterson
November 17, 2025 AT 08:31Interesting breakdown. I’d add that insulin resistance isn’t just about diet - it’s also about chronic stress. Cortisol elevates blood glucose and promotes visceral fat storage. Many people focus on macros but ignore sleep and mental load. A person eating clean but working 70-hour weeks and sleeping 4 hours? Still insulin resistant. The body doesn’t care if your plate looks perfect - it cares if you’re in fight-or-flight mode 24/7. That’s the silent driver.
Also, the shift from 'metabolic syndrome' to 'metabolic dysfunction syndrome' is overdue. The old term made it sound like a checklist. The new one reflects the systemic failure - which is more accurate and less stigmatizing. Labels matter.
Jessica M
November 17, 2025 AT 09:23Thank you for this exceptionally well-researched and clearly articulated overview. The integration of clinical data with actionable lifestyle recommendations is precisely what is missing from most public health messaging. I would like to emphasize that the reversal of insulin resistance is not only possible but is, in fact, a well-documented physiological phenomenon supported by over three decades of peer-reviewed literature. The Diabetes Prevention Program remains one of the most robust interventions in preventive medicine, demonstrating that behavioral modification can outperform pharmacological intervention in both efficacy and durability. Furthermore, the emphasis on waist circumference as a biomarker is critical - it is a more sensitive indicator of metabolic risk than BMI, particularly in non-obese populations. I urge all readers to consult with a qualified healthcare provider before initiating any new regimen, and to prioritize evidence-based interventions over trending fads. The science is clear. The path forward is accessible. The time to act is now.
Erika Lukacs
November 18, 2025 AT 21:57It’s strange how we’ve turned biology into a problem to be solved rather than a system to be understood. We want to fix insulin resistance like a broken machine, but maybe it’s not broken - maybe it’s trying to survive in a world that no longer makes sense to it. We feed it sugar, then punish it for not handling it. We tell it to move more, but never ask why it’s so tired. Maybe the question isn’t how to reverse it - but how to stop breaking it in the first place.
Rebekah Kryger
November 19, 2025 AT 08:11Everyone’s obsessed with 'reversing' insulin resistance like it’s a glitch. But here’s the jargon you’re not hearing: adipocyte hypertrophy, ectopic lipid deposition, and ceramide-induced serine phosphorylation of IRS-1. That’s the real mechanism. You can’t fix it with kale and walks - you need to understand the molecular cascade. And no, Ozempic isn’t magic - it’s a GLP-1 receptor agonist that enhances insulin secretion and suppresses glucagon. But you don’t need to know that, do you? You just want a quick fix. That’s why you’re still here.
Victoria Short
November 20, 2025 AT 09:51eh. sounds like a lot of work.
Eric Gregorich
November 20, 2025 AT 12:36Let me tell you something - I was diagnosed with prediabetes at 34. I was 190 pounds, ate like a teenager, and thought ‘I’m young, I’ve got time.’ I didn’t believe this stuff until my HbA1c hit 6.1%. Then I started walking after dinner. Not for ‘fitness.’ Just to move. And I stopped drinking soda. Not because I ‘knew better’ - because I was tired of feeling like a zombie after lunch. Four months later, my HbA1c was 5.4%. I didn’t lose 20 pounds. I lost 8. But my energy? It came back. Like someone flipped a switch. And you know what? I didn’t take a pill. I didn’t join a program. I just stopped making my body suffer for my convenience. And now? I don’t think of it as ‘reversing’ anything. I think of it as finally listening. Your body doesn’t need a revolution. It just needs you to stop screaming at it with sugar and stress.
Koltin Hammer
November 21, 2025 AT 12:46There’s a deeper layer here that nobody’s talking about - and it’s not just about glucose or fat. It’s about rhythm. Our ancestors didn’t eat three meals a day. They ate when they found food. They moved when they had to. They slept when the sun went down. We’ve replaced natural cycles with clocks and convenience. We’re not just eating wrong - we’re living wrong. The body evolved to thrive in uncertainty - feast and famine, movement and rest. Now we live in constant abundance and constant motion. No peaks. No valleys. Just flatline. And our metabolism? It’s screaming for a storm. But we’re giving it a spreadsheet.
That’s why people who eat ‘healthy’ still get metabolic syndrome. Because they’re still in the same cage - just with kale instead of fries. The solution isn’t just what you eat - it’s how you live. Wake up at dawn. Eat with the sun. Move without a goal. Sleep without an alarm. Let your body remember how to be alive, not just survive.
And maybe - just maybe - insulin resistance isn’t a disease. It’s a protest.
Phil Best
November 22, 2025 AT 05:19Oh, so now I’m supposed to walk 150 minutes a week and eat ‘whole grains’ while my boss gives me a ‘wellness stipend’ of $50 a year? And you think I’m gonna do that while working 60 hours and my kid has soccer practice? You know what’s easier than reversing insulin resistance? Getting a prescription for Ozempic and pretending you’re a biohacker. At least then you get to lose weight and feel smug about it. Meanwhile, I’ll be here, eating a burrito at 11 p.m., wondering why my body hates me. Spoiler: it doesn’t. It just knows I’m not worth the effort.
Parv Trivedi
November 22, 2025 AT 12:02This is beautiful. I come from India, where many people are thin but still have high blood sugar. We call it 'sweet blood' - but no one talks about why. The truth? Our bodies were built for rice and lentils, not pizza and soda. My grandmother never ate sugar - but she lived to 92. She walked to the market every day. She ate what was grown nearby. She didn’t count calories. She listened to her body. We lost something when we traded wisdom for labels. This post reminds me of her. Thank you.
Brendan Peterson
November 22, 2025 AT 12:58That’s actually really well put, Parv. I’ve seen the same thing in my family - my uncle is lean, eats rice daily, but his HbA1c is 7.2%. He never had a chance to know about insulin resistance. He just thought he was ‘getting old.’ The cultural shift away from traditional diets is a silent epidemic. It’s not just about food - it’s about identity. When you lose your food culture, you lose your metabolic rhythm.