Managing Menstrual Migraines: Practical Relief Strategies
If you get pounding headaches right before or during your period, you’re not alone. Many women call them "period migraines" and they can ruin daily plans. The good news? A few everyday moves can cut the pain down dramatically.
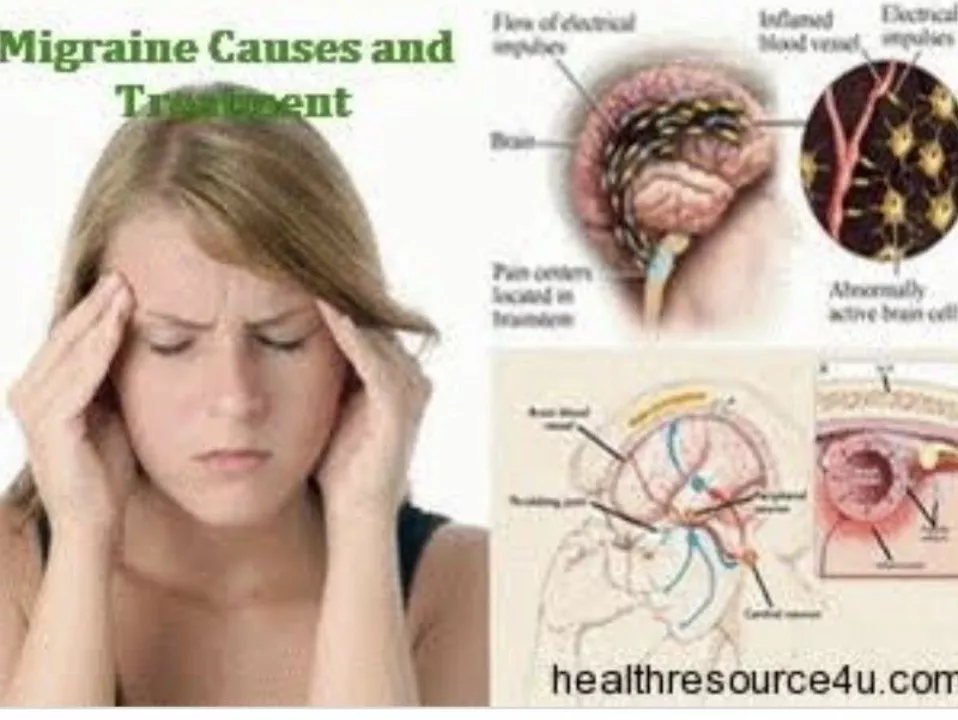
Why Hormones Trigger Headaches
Your body’s hormone roller‑coaster is the main culprit. Estrogen drops a day or two before menstruation, then spikes again when bleeding starts. Those rapid shifts affect blood vessels in the brain and can spark a migraine. Knowing this link helps you plan ahead.
Start by noting exactly when the pain hits each month. A simple calendar or phone app works – jot down headache start, intensity, and any triggers like lack of sleep or certain foods. After a few cycles you’ll see patterns and can time your preventive steps.
Quick Ways to Ease the Pain
Over‑the‑counter painkillers such as ibuprofen or naproxen work for many women if taken early, before the headache peaks. Don’t wait until you’re already in a throbbing zone – set an alarm for the day your symptoms usually begin.
Hydration matters more than you think. Dehydration narrows blood vessels and can amplify migraine signals. Keep a water bottle handy and aim for at least eight glasses a day, especially when you know your period is near.
Caffeine can be a double‑edged sword. A small cup of coffee or tea early in the headache may give relief, but too much later can cause rebound headaches. If you’re sensitive, stick to one cup and watch how you feel.
Magnesium supplements (200–400 mg daily) have solid anecdotal support for menstrual migraine relief. Look for magnesium citrate or glycinate – they’re easier on the stomach. Pair this with riboflavin (vitamin B2) at 400 mg a day and you might notice fewer attacks.
Sleep is your secret weapon. Aim for consistent 7‑8 hours each night, and try to keep bedtime regular even on weekends. A short nap (20 minutes) early in the day can also reset pain pathways before they flare.
Stress builds tension that feeds migraines. Simple breathing exercises, a quick walk, or gentle yoga stretches can calm nerves fast. Even five minutes of focused breathing – inhale for four counts, hold two, exhale four – often eases the pressure.
If OTC meds and lifestyle tweaks aren’t enough, talk to your doctor about prescription options. Triptans such as sumatriptan are proven migraine relievers and can be used specifically for menstrual attacks. Hormonal birth control pills or a hormonal IUD may smooth out estrogen swings altogether, reducing headache frequency.
For long‑term prevention, start any preventive measure a few days before your typical migraine window. This could mean taking magnesium, a low dose of ibuprofen, or using a triptan as a “pre‑emptive” dose. Consistency is key – the body responds best when you keep a steady routine.
Bottom line: menstrual migraines are manageable with a mix of tracking, early medication, hydration, sleep, and smart supplements. Try one change at a time, note what works, and adjust as needed. If headaches persist or worsen, get professional help – there’s always another option waiting.
As someone who suffers from menstrual migraines, I've recently discovered the benefits of dydrogesterone in managing these painful headaches. Dydrogesterone, a synthetic progesterone, can help stabilize hormonal fluctuations that often trigger menstrual migraines. By maintaining a consistent hormonal balance, dydrogesterone effectively reduces the frequency and severity of these migraines. I've personally experienced significant relief since incorporating this treatment into my routine. It's certainly worth discussing with your healthcare provider if you suffer from debilitating menstrual migraines.

 Medications
Medications