Why Storage Matters for Liquid Antibiotics
When you pick up a bottle of liquid antibiotic for your child, it might look like just another medicine. But the truth is, how you store it can make the difference between healing and a lingering infection. Liquid antibiotics, especially those mixed from powder, are fragile. Too much heat, too much cold, or just too much time, and they can lose their power. The FDA says expiration dates only mean something if the drug was stored the right way. If you leave it on the windowsill or forget to refrigerate it, you might be giving your child medicine that doesn’t work.
Refrigeration: Not Always Required
A lot of people assume all liquid antibiotics need to go in the fridge. That’s not true. Some do. Some don’t. And some can actually break down if chilled.
Amoxicillin, one of the most common antibiotics for kids, can be stored either in the fridge (between 2°C and 8°C) or at room temperature (20°C to 25°C). The Cleveland Clinic says it’s fine either way - but if you keep it at room temperature, you’ll need to use it faster. Refrigeration helps it last longer, but it’s not mandatory.
On the other hand, amoxicillin-clavulanate (also called co-amoxiclav) is trickier. While some sources say it should be refrigerated and used within 10 days, others say it’s stable for up to 14 days at room temperature. The key? Always check the label. The manufacturer tested this specific batch under specific conditions. Their instructions override general advice.
Some antibiotics, like certain formulations of erythromycin or azithromycin, can actually become less effective if refrigerated. Cold temperatures can cause the active ingredients to separate or clump. That’s why Walgreens pharmacists warn: refrigerating certain liquid antibiotics makes them weaker. Don’t guess. Read the box.
How Long Do They Last After Mixing?
Once you mix the powder with water, the clock starts ticking. Unlike pills that last years, reconstituted suspensions have short lives.
For amoxicillin, most manufacturers say you can keep it for up to 14 days - whether it’s in the fridge or on the counter. But if you’re using amoxicillin-clavulanate, the clavulanate part degrades faster than the amoxicillin. A 2013 study found that even at room temperature (27-29°C), it stayed stable for five days. After that, the clavulanate loses strength, which means the antibiotic won’t fight resistant bacteria as well.
Don’t rely on how it looks. If it’s still clear and smells okay, you might think it’s fine. But degradation happens at a molecular level. You can’t see it. That’s why the rule is simple: when in doubt, throw it out. If it’s past the date on the bottle, or if you’re unsure how long it’s been out, don’t risk it.
What Happens If You Store It Wrong?
Improper storage doesn’t make antibiotics dangerous - it makes them useless.
When antibiotics lose potency, they don’t kill all the bacteria. The weak ones die. The strong ones survive. Those survivors multiply. That’s how antibiotic resistance starts. A child with an ear infection might seem to get better at first, then get sick again - not because the infection came back, but because the medicine didn’t work.
Baystate Health reports that about 30% of households store medications incorrectly. Common mistakes: leaving medicine on the bathroom counter (heat and steam), keeping it in the car (freezing in winter, baking in summer), or storing it near the stove or radiator. Even sunlight can break down the chemicals. One study found that liquid antibiotics stored on open shelves in homes with poor cooling had significantly reduced potency.
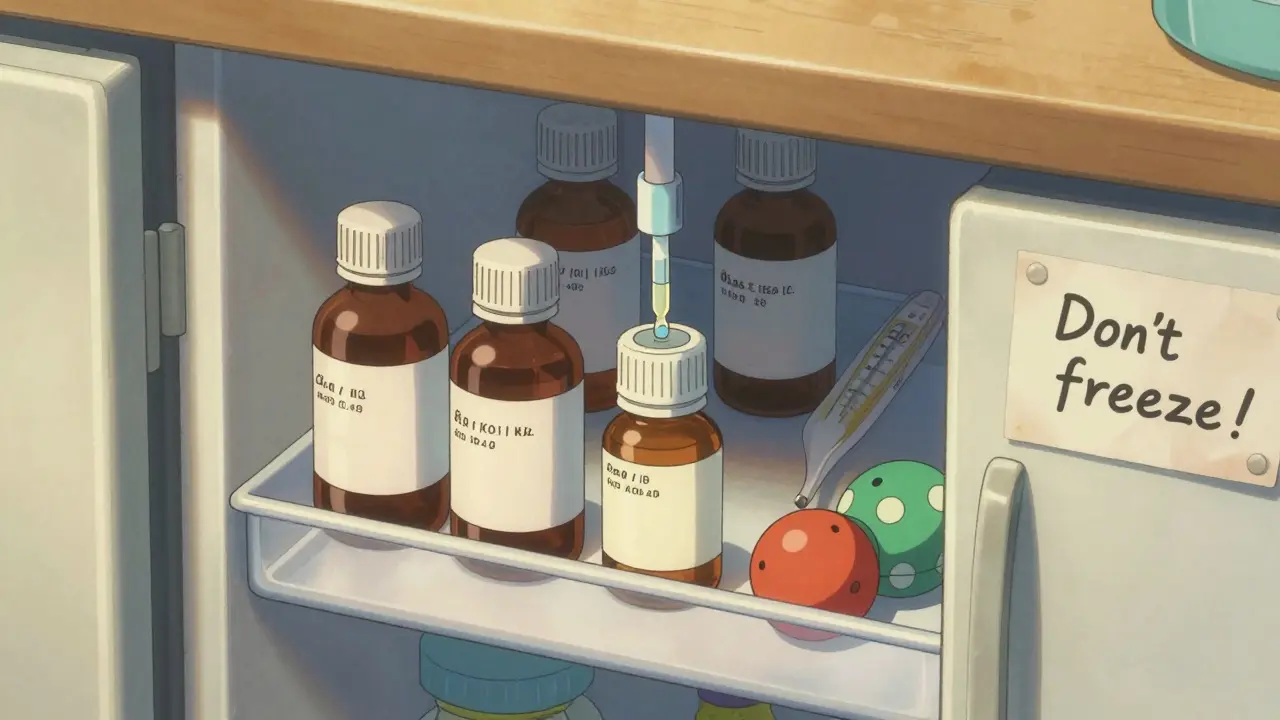
And don’t freeze it. Freezing can destroy the structure of the suspension. It’s not just about antibiotics - insulin, hormones, and other protein-based drugs can be ruined by freezing. The same principle applies here.
How to Store Them Right
- Read the label. Every bottle has storage instructions. Look for phrases like “store in refrigerator,” “keep at room temperature,” or “discard after 14 days.”
- Use the original container. Don’t pour it into a different bottle. The original packaging protects it from light and keeps the label with expiration and storage info.
- Keep it away from light. Sunlight, even through a window, can degrade the medicine. Store it in a cupboard, not on the counter.
- Avoid extreme temperatures. Don’t leave it in the car, near the oven, or in a cold garage. The ideal spot is a cool, dry place - like a bedroom drawer or kitchen cabinet away from the sink.
- Use a measuring device. Never use a kitchen spoon. Use the syringe, dropper, or cup that came with it. A teaspoon is not the same as a medicine teaspoon. Inaccurate dosing leads to under-treatment or side effects.
- Shake well before each use. Suspensions settle. The medicine sinks to the bottom. If you don’t shake it, you might give your child a dose with too little or too much active ingredient.
Traveling With Liquid Antibiotics
If you’re flying or driving with a reconstituted antibiotic, plan ahead.
For refrigerated meds: Use a small insulated cooler with a cold pack. Don’t let the bottle freeze. Wrap the cold pack in a towel so it doesn’t touch the bottle directly. If you’re on a long trip and can’t keep it cool, ask your pharmacist if the antibiotic is stable at room temperature. Some newer formulations are designed for this.
For room-temperature meds: Keep them in your carry-on. Don’t check them in luggage. Temperatures in airplane cargo holds can drop below freezing or rise above 40°C. That’s dangerous for any medicine.
Always carry the original label. If you’re questioned at security or by a doctor abroad, the label proves it’s legitimate and shows proper storage conditions.

What to Do With Expired or Unused Antibiotics
Never flush them down the toilet or throw them in the trash. That pollutes water and can lead to environmental antibiotic resistance.
In the UK, most pharmacies offer free medicine take-back programs. Take your unused liquid antibiotics to your local pharmacy. They’ll dispose of them safely.
If there’s no take-back program nearby, mix the liquid with something unappealing - coffee grounds, cat litter, or dirt - pour it into a sealed container, and throw it in the bin. Remove the label or black it out so no one knows what it was.
And never save leftover antibiotics for next time. Bacteria change. The infection might be different. Giving the wrong antibiotic can delay proper treatment.
When in Doubt, Ask
Pharmacists are your best resource. They know the exact stability data for the brand you got. If the label is faded, or you’re unsure if the medicine is still good, call the pharmacy. They can tell you if it’s safe to use.
Don’t rely on memory. Don’t assume all antibiotics work the same. A bottle of amoxicillin isn’t the same as a bottle of cephalexin. One might need refrigeration. The other might not. One lasts 14 days. The other only 7.
Proper storage isn’t just about following rules. It’s about making sure your child gets the full benefit of the medicine - and helping stop the rise of antibiotic-resistant superbugs.
Quick Checklist for Safe Storage
- ☑️ Read and follow the label instructions
- ☑️ Store in original container
- ☑️ Keep away from heat, light, and moisture
- ☑️ Never freeze
- ☑️ Shake before each dose
- ☑️ Use correct measuring tool
- ☑️ Discard after the stated time (usually 7-14 days)
- ☑️ Return unused medicine to pharmacy


 Medications
Medications
Keith Helm
January 22, 2026 AT 07:38- Keith Helm
Rob Sims
January 23, 2026 AT 12:13arun mehta
January 24, 2026 AT 16:40Philip House
January 25, 2026 AT 01:46Jasmine Bryant
January 25, 2026 AT 09:18shivani acharya
January 26, 2026 AT 22:58Brenda King
January 28, 2026 AT 18:51Tatiana Bandurina
January 29, 2026 AT 18:13Daphne Mallari - Tolentino
January 30, 2026 AT 03:49