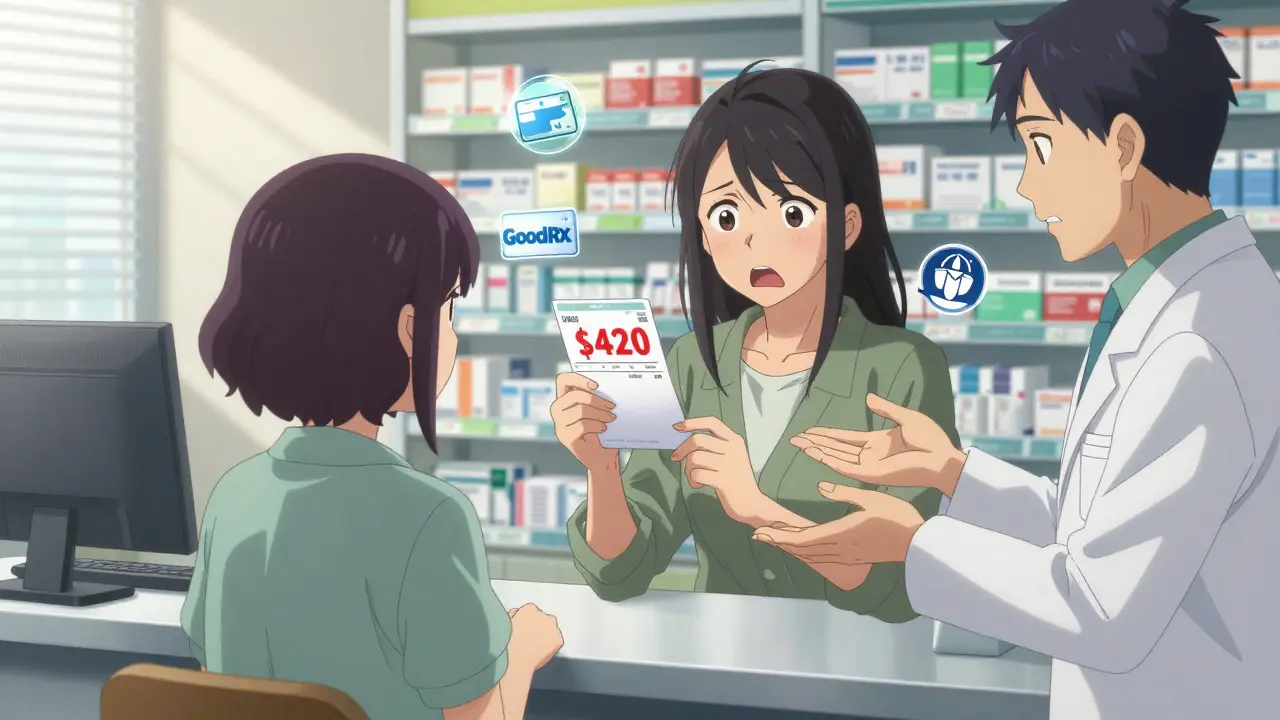
Imagine this: you leave your doctor’s office with a new prescription, feeling hopeful about your treatment. But when you get to the pharmacy, the pharmacist tells you the copay is $420. You freeze. You didn’t sign up for this. You didn’t even know it could cost this much. This happens to 22% of people in the U.S. every year - they walk away from their prescriptions because they can’t afford them. It doesn’t have to be this way.
Why Talking About Cost Before You Get the Script Matters
Most people assume their insurance will cover their meds, or that the doctor knows the price. But that’s not always true. Insurance plans change every year. Formularies - the lists of drugs they cover - shift constantly. A drug covered last year might be moved to a higher tier this year, or dropped entirely. And if you’re on Medicare, Medicaid, or a marketplace plan, your out-of-pocket costs can vary wildly.The good news? You don’t have to guess. Studies show that when patients talk about cost before the prescription is written, they’re 37% less likely to skip doses or skip refills because of price. That’s not a small number. It’s life-changing.
Starting in 2026, Medicare Part D beneficiaries won’t pay more than $2,100 out-of-pocket for all their prescription drugs in a year. That’s a huge shift. But even with this cap, you still need to know what you’re getting into. Why? Because if you don’t plan ahead, you might hit that cap early and still pay full price for everything else - or worse, miss doses while you’re figuring it out.
What You Need to Know Before Your Appointment
Don’t wait until you’re in the pharmacy to ask questions. Prepare before your doctor’s visit. Here’s what to do:- Check your plan’s formulary. Every insurance company has a list of covered drugs. Log into your plan’s website (Medicare.gov for Part D, or your insurer’s portal) and search for your medication. Look for the tier it’s on - Tier 1 (generic) usually costs $5-$15, Tier 2 (preferred brand) $25-$50, and Tier 3 or specialty can be $50-$100 or more.
- Know your deductible. If you haven’t met your deductible this year, you might pay full price until you do. For individual marketplace plans in 2023, the average deductible was $480. If you’re early in the year (January-March), that’s when costs hit hardest.
- Find out if you’re on a payment plan. Medicare Part D now offers a Prescription Payment Plan starting in 2025. Instead of paying $300 at once, you can pay $25/month. But you have to enroll early - if you sign up in October, you get 12 months to spread it out. If you wait until November? You only get 2 months. That’s not a mistake - it’s a trap.
- Check for insulin and vaccine caps. Under the Inflation Reduction Act, insulin costs are capped at $35/month for Medicare users. Vaccines like flu shots and shingles are now free. Don’t assume - confirm.
What to Say to Your Doctor
Your doctor wants you to take your medicine. They just might not know how much it costs. So lead the conversation.Use phrases like:
- “I’m worried about the cost of this medication. Is there a generic version?”
- “I’m on a fixed income. Can we look at alternatives that are covered under my plan?”
- “I’ve heard about the $2,100 out-of-pocket cap for Medicare. Does this drug count toward that?”
- “Can you check if this is on my plan’s formulary before writing the script?”
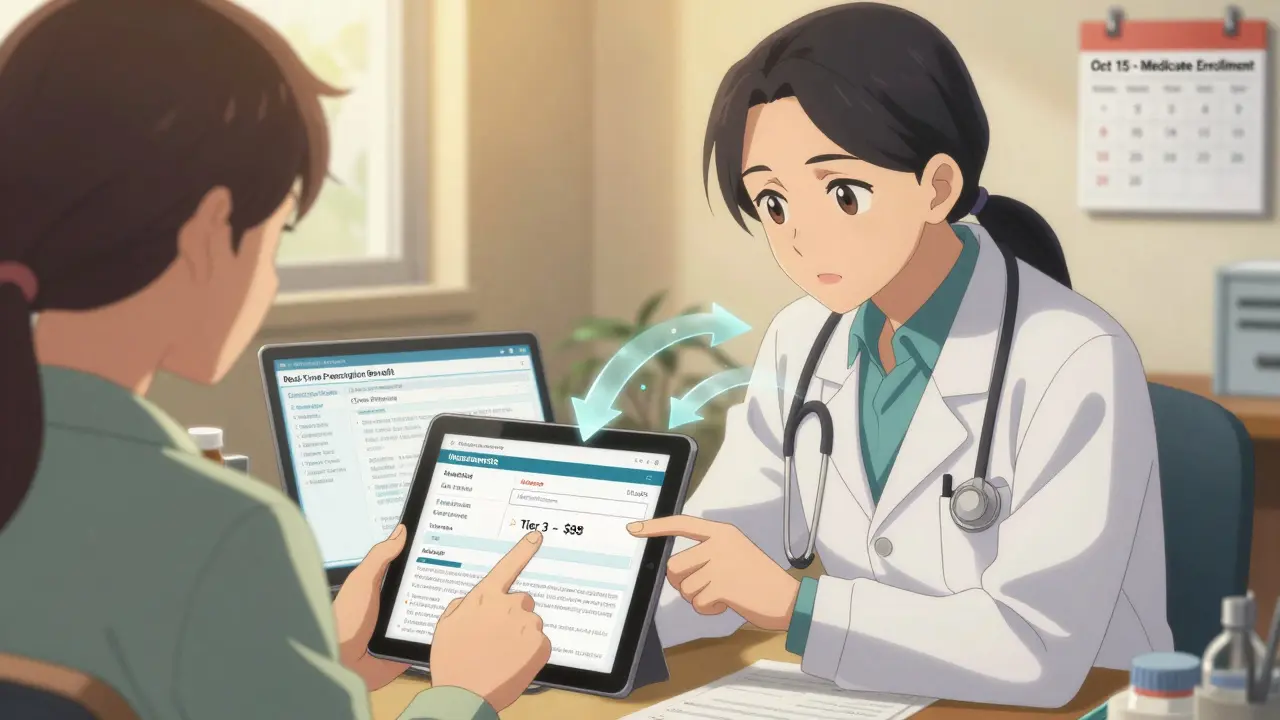
Doctors can use tools like Surescripts’ Real-Time Prescription Benefit (RTPB), which shows up in electronic health records. If your doctor says they don’t have access to that, ask them to call the pharmacy or your insurer. It’s their job to help you navigate this.
What to Ask the Pharmacist
Pharmacists are your last line of defense. They know what’s covered, what’s not, and what alternatives exist. Don’t just hand over the script and walk away.Ask:
- “What’s my out-of-pocket cost today?”
- “Is there a generic or therapeutic alternative?”
- “Can I use a mail-order service to save money?”
- “Do you have a discount card? I’ve heard of GoodRx - can you compare it to my insurance?”
One patient in Melbourne saved $287 on blood pressure meds by showing her pharmacist a GoodRx price - and her insurance still covered it. That’s possible because pharmacies often accept discount cards even when insurance doesn’t cover the full cost. It’s not cheating. It’s smart.
How Insurance Types Compare
Not all coverage is the same. Here’s what you’re likely dealing with:| Insurance Type | Out-of-Pocket Cap | Copay Range | Specialty Drug Costs | Key Advantage |
|---|---|---|---|---|
| Medicare Part D | $2,100 (2026) | $5-$100 per fill | Up to 33% coinsurance, but capped at $2,100 total | Hard annual limit, insulin at $35/month |
| Medicaid | None (state-dependent) | $1-$3 | Often requires prior authorization | Lowest copays, covers all FDA-approved drugs |
| Commercial (Marketplace) | No federal cap | $15-$150+ per fill | Up to 50% coinsurance, no limit | More drug choices, but unpredictable costs |
Commercial plans are the most confusing. They can have 5 or 6 tiers. One drug might be covered under one plan but not another. And there’s no cap on how much you pay - unless you’re lucky enough to have an employer that sets one. That’s why checking your formulary before every refill is non-negotiable.
Tools That Actually Work
You don’t need to be an expert to save money. These tools are free and reliable:- Medicare.gov Plan Finder - Updated every October. Compare up to 28 drugs across plans. Use it during Annual Enrollment Period (Oct 15-Dec 7).
- GoodRx - Shows cash prices and discount coupons. Used by 70% of people looking for drug savings. Works even if you have insurance.
- CVS Caremark’s Check Drug Cost Tool - If your plan uses Caremark, use their website. It pulls your real-time coverage data.
- Call Your Insurance - Have your NDC (National Drug Code) ready. It’s on the pill bottle. Ask: “What’s my cost today, with my deductible status?”
Pro tip: Don’t trust the price you see on your insurance website. It’s often outdated. Always call the pharmacy or insurer directly before filling.

What to Do If Your Drug Isn’t Covered
If your medication isn’t on the formulary, don’t give up. There are two paths:- Prior Authorization - Your doctor submits paperwork to your insurer, explaining why you need this drug. This works in 68% of cases, according to 2023 data from the Department of Managed Health Care.
- Therapeutic Alternative - Ask your doctor: “Is there another drug in the same class that’s covered?” For example, if you’re on a brand-name statin, there are 5 generics that work just as well.
One patient in Melbourne had her $1,200/month medication switched to a generic after her doctor used the RTPB tool during the visit. She saved $14,400 a year. That’s not luck - it’s preparation.
When to Act - Timing Matters
Timing isn’t just about when you take the pill. It’s about when you ask.- Before your appointment - Review your formulary and deductible.
- During your visit - Ask your doctor to check coverage.
- Before leaving the pharmacy - Ask for the final cost and compare it to GoodRx.
- October-December - Use this window to switch Medicare plans if needed.
If you wait until you’re at the counter, you’ve already lost control of the situation.
What’s Changing in 2025-2026
The rules are shifting fast. Here’s what’s new:- Medicare Part D out-of-pocket cap: $2,100 (down from $8,000 in 2024)
- Insulin: $35/month, no matter your income
- All Part D plans must offer monthly payment plans by 2025
- Real-Time Prescription Benefit tools will be required in all certified EHRs by 2026
This isn’t just policy - it’s a lifeline. But only if you know how to use it.
Can I use GoodRx even if I have insurance?
Yes. Many pharmacies accept GoodRx coupons even if you have insurance. Sometimes the cash price with GoodRx is lower than your insurance copay. Always ask the pharmacist to compare both. You can’t use both at once, but you can choose the cheaper option.
What if my doctor won’t discuss cost?
If your doctor dismisses your concerns, ask for a referral to a pharmacist or patient advocate. Many hospitals have financial counselors who help with medication costs. You can also call the Patient Advocate Foundation’s helpline - they help resolve coverage issues in over 68% of cases. Your health shouldn’t depend on your doctor’s willingness to talk about money.
Do all pharmacies accept discount cards?
Most major chains - CVS, Walgreens, Rite Aid, Kroger - accept discount cards like GoodRx, SingleCare, and RxSaver. Smaller pharmacies may not, but you can often call ahead. If they don’t accept it, ask if they can order the drug at the cash price. Many will.
Why does my cost change every month?
If you’re on a commercial plan, your out-of-pocket costs depend on your deductible, coinsurance, and whether you’ve hit your out-of-pocket maximum. Medicare Part D costs are more stable once you’re past the deductible, but specialty drugs can still vary. Always check your plan’s formulary each year - changes happen without notice.
Can I switch Medicare plans mid-year?
Only under special circumstances - like moving out of your plan’s service area, losing employer coverage, or qualifying for Extra Help. Otherwise, you must wait until October-December for the Annual Enrollment Period. But if you’re facing unaffordable costs, contact Medicare to ask about a Special Enrollment Period. It’s not guaranteed, but it’s worth asking.
Prescription costs shouldn’t be a surprise. You have the right to know what you’re paying for - and the power to change it. Start the conversation before the script is written. Ask the questions. Use the tools. Save your money. And your health.

 Medications
Medications