Medication Desensitization Dosing Calculator
Desensitization Dosing Calculator
Calculate your dose progression schedule for rapid medication desensitization protocols used for immediate allergic reactions.
When a medication saves your life but also triggers a dangerous allergic reaction, what do you do? For many patients, the answer isn’t stopping treatment-it’s desensitization. This isn’t a miracle cure or a shortcut. It’s a carefully controlled medical process that lets people who’ve had severe allergic reactions safely take life-saving drugs they were once told to avoid forever.
What Desensitization Actually Does
Desensitization doesn’t fix your allergy. It doesn’t change your immune system permanently. Instead, it temporarily tricks your body into tolerating the drug long enough to get through a course of treatment. Think of it like slowly turning up the volume on a speaker that’s too loud-you don’t make the sound quieter, you just teach your ears to handle it for a while.
This technique was developed in the 1960s at the National Institutes of Health and later refined by Dr. Mariana Castells at Brigham and Women’s Hospital. Today, it’s used in hospitals worldwide, especially when no other drug works. For example, if you’re allergic to penicillin but have a bone infection that only responds to it, desensitization might be your only option.
Success rates are high-95% to 100%-when done correctly under medical supervision. Patients with severe penicillin allergies have completed full antibiotic courses after desensitization with no life-threatening events. In cancer care, patients who react to taxanes like paclitaxel often get their chemotherapy through desensitization instead of switching to less effective drugs.
When Is It Used? The Three Key Scenarios
Desensitization isn’t for every allergic reaction. It’s reserved for three specific situations:
- No safe alternative exists. Some infections or cancers respond only to one drug. If you’re allergic to that drug, and no other works, desensitization is the only path forward.
- The drug is significantly more effective. For example, carboplatin might be less effective than cisplatin for ovarian cancer. If you’re allergic to cisplatin but it’s your best shot, desensitization lets you use it.
- The reaction is IgE-mediated (immediate). This means symptoms like hives, swelling, trouble breathing, or drop in blood pressure happen within minutes to an hour after exposure. These are the reactions desensitization works best for.
It’s not used for delayed reactions like rashes that appear days later, and it’s strictly avoided in cases of Stevens-Johnson syndrome or toxic epidermal necrolysis-severe skin reactions where the risk of death is too high.
Two Types of Protocols: Fast and Slow
There are two main ways to do desensitization, chosen based on the type of reaction and the drug:
Rapid Drug Desensitization (RDD)
RDD is the most common. It’s used for immediate reactions and typically takes 4 to 6 hours. The process starts with a dose so tiny-1/10,000th of the full therapeutic amount-that it doesn’t trigger a reaction. Then, every 15 minutes, the dose is doubled until the full dose is reached.
For IV antibiotics like penicillin or vancomycin, this means 12 carefully calculated steps. Nurses monitor blood pressure, oxygen levels, and breathing after each dose. If a mild reaction like flushing or itching happens, they pause, give antihistamines, and continue. Severe reactions are rare-under 2%-when protocols are followed exactly.
Slow Drug Desensitization (SDD)
SDD is used for delayed reactions, like those caused by some chemotherapy drugs or aspirin. It’s slower because it targets T-cells, not IgE antibodies. Instead of doubling doses every 15 minutes, doses are given hours or even days apart.
Aspirin desensitization, for example, can take two to three days. Patients start with a few milligrams and slowly increase, waiting at least 60 minutes between oral doses. This is often done in outpatient clinics but still requires an allergist’s oversight.
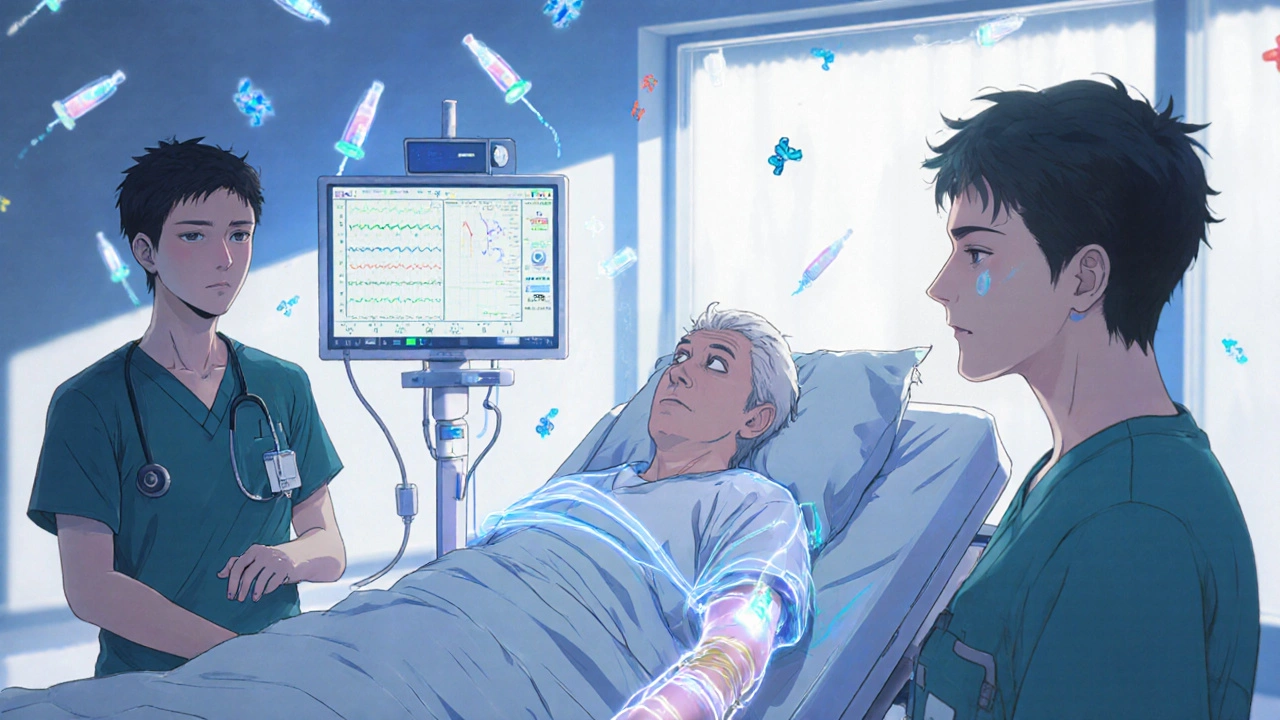
What Happens During the Procedure?
Desensitization isn’t something you can do at home. It requires:
- A hospital or specialized clinic with anaphylaxis-ready equipment
- An allergist or immunologist present the whole time
- Nursing staff trained in emergency response
- Continuous monitoring: blood pressure, heart rate, oxygen levels, and lung sounds
Before starting, the team reviews your history. Did you have anaphylaxis? Did you need epinephrine? Was it a skin rash or breathing trouble? This determines if you’re even a candidate.
During the process, you’ll be in a room with emergency meds on standby-epinephrine, steroids, IV fluids. If you react, they stop the infusion, treat you, and decide whether to continue. Most mild reactions are manageable and don’t stop the process.
After you reach the full dose, you stay for another hour to make sure nothing happens. Then, you can go home-but only if you’re stable.
Why It Beats Alternatives
Some doctors try premedication-giving antihistamines or steroids before the drug. But this doesn’t work well. In one study, 10% of cancer patients still had severe reactions to taxanes even with premedication. Desensitization cut that risk to under 2%.
Switching drugs sounds safer, but it’s not always possible. Cross-reactivity between penicillins and cephalosporins happens in 15-20% of cases. If you’re allergic to one, you might react to the other too. Desensitization lets you use the drug you need, not the one you’re least likely to react to.
And in the age of antibiotic resistance, it’s becoming more critical. The CDC reports 35,000 deaths a year in the U.S. from drug-resistant infections. Many of those patients could be treated with antibiotics they’re allergic to-if they could be desensitized.
The Catch: It’s Temporary and Resource-Heavy
Here’s the big limitation: desensitization only works while you’re getting the drug. If you stop the medication for more than 48 hours, your body forgets the tolerance. You’ll need to go through the whole process again for the next course.
That’s why it’s not used for long-term daily drugs like aspirin for heart disease-unless you have a specific condition like aspirin-exacerbated respiratory disease.
It’s also expensive and time-consuming. Each IV desensitization takes 4.2 nursing hours and 1.8 physician hours. Smaller hospitals often can’t justify the staff or equipment. That’s why it’s most common in academic centers-where 85% of eligible patients get it-and rare in community hospitals, where only 35% do.
Errors happen too. In 8% of cases, the drug is prepared wrong. In 15% of cases, the wrong patient is selected. That’s why standardized kits and electronic checklists are now standard in top centers. Simulation training has cut protocol errors from 22% to under 5%.
Real Patient Stories
One patient, u/PenicillinWarrior on Reddit, had been told for 20 years that he couldn’t take penicillin after a childhood rash. When he developed osteomyelitis, the only effective antibiotic was penicillin. He went through a 4-hour RDD protocol and completed his treatment. “I finally got the right treatment,” he wrote. “No more guessing.”
Another, u/ChemoSurvivor, had a rough start. “My hospital didn’t have the right dilution kits,” she said. “It took three tries before they got it right.” That’s why standardized protocols matter. A single mistake can delay treatment or cause harm.
On the flip side, 92% of oncology patients who’ve been through it say it was “life-saving.” The anxiety is real-63% report feeling terrified before the procedure-but most say it was worth it.
What’s Next for Desensitization?
The field is evolving fast. In 2023, the American Academy of Allergy, Asthma & Immunology released standardized national protocols, ending years of confusion between different hospital methods.
New research is looking at biomarkers-like basophil activation tests-that can predict success with 89% accuracy. Imagine knowing before you start whether your body will respond. That’s coming soon.
Home-based desensitization is being tested in phase 2 trials. For stable patients who’ve already completed one cycle, doctors are exploring whether they can safely continue at home under remote monitoring. Early results show 92% success.
Long-term, experts believe genetic and immune profiling will guide who needs desensitization and which protocol to use. Within five years, your allergy history might be paired with your immune profile to create a personalized plan.
Final Thoughts
Desensitization isn’t a first-line solution. It’s a last-resort tool that saves lives when no other option exists. It’s not risk-free, but the risks are far lower than the consequences of not treating a serious infection or cancer.
For patients, it means regaining control. No more being labeled “allergic to everything.” No more settling for weaker drugs. Just the chance to get the treatment that works.
For doctors, it means mastering a complex, high-stakes procedure. It’s not something you learn from a textbook. You need hands-on training, supervision, and a team ready to respond.
And for the healthcare system? It’s a necessary investment. As antibiotics fail and cancer drugs get more complex, desensitization will become less of a specialty trick-and more of a standard part of care.
Can I do desensitization at home?
No, not currently. Desensitization requires constant medical monitoring, emergency equipment, and trained staff. Even mild reactions can turn dangerous quickly. While home-based protocols are being tested in clinical trials, they’re not approved for general use yet. All current procedures must be done in a hospital or specialized allergy clinic.
How long does a desensitization take?
It depends on the drug and method. Rapid desensitization for IV antibiotics usually takes 4 to 6 hours. Oral desensitization for aspirin or NSAIDs can take 2 to 3 days, with doses spaced hours apart. Slow desensitization for chemotherapy drugs may be spread over several days with daily visits. The full process includes monitoring before, during, and after the final dose.
Does desensitization work for all types of allergic reactions?
No. It works best for immediate, IgE-mediated reactions-like hives, swelling, trouble breathing, or anaphylaxis that happens within minutes. It’s not effective for delayed reactions like rashes that appear days later, and it’s dangerous for severe skin reactions like Stevens-Johnson syndrome or toxic epidermal necrolysis. These require completely different management.
Will I be allergic to the drug forever after desensitization?
No. Desensitization creates temporary tolerance. If you stop taking the drug for more than 48 hours, your body loses the tolerance. You’ll need to repeat the entire process for the next course. It doesn’t cure the allergy-it just lets you take the drug safely while you’re on it.
Is desensitization covered by insurance?
It depends. Medicare and some private insurers cover desensitization when it’s medically necessary, but reimbursement often covers only about 60% of the actual cost. This creates financial pressure on hospitals, especially smaller ones, which may not have the resources to offer it. Always check with your provider and ask for pre-authorization.

 Medications
Medications
Tanuja Santhanakrishnan
October 30, 2025 AT 06:23Wow, this is one of those posts that makes you realize how much medicine has evolved without most of us noticing. I work in a rural clinic, and we get patients all the time who’ve been told they can’t take penicillin after a rash at age 5-now they’re septic and we’re stuck. Desensitization isn’t magic, but it’s the closest thing we’ve got to turning a dead end into a lifeline. Kudos to the teams making this happen.
Glenda Walsh
October 30, 2025 AT 11:50Wait-so you’re telling me… people are getting chemo after being told they’re allergic… and they don’t just stop? I mean, what if they react mid-infusion? Like, what if the nurse messes up the dilution? I’ve seen too many horror stories… this feels like playing Russian roulette with a syringe.
Karen Werling
November 1, 2025 AT 03:49My aunt went through this for paclitaxel last year. She was terrified. We all were. But the nurses were so calm, so precise-it felt like watching a ballet. She got through it. Now she’s back to hiking. I just wish more hospitals had this kind of care. Not everyone lives near a big academic center.
Emil Tompkins
November 1, 2025 AT 03:59So this is just another way Big Pharma keeps people hooked? They make drugs that cause reactions, then charge you thousands to un-break your body so you can keep taking the poison? And they call it ‘medicine’? I’ve seen the data-these protocols are barely tested. This is a money racket disguised as science.
Raj Modi
November 2, 2025 AT 15:01From an immunological standpoint, the distinction between IgE-mediated and T-cell-mediated reactions is absolutely critical in determining protocol selection. The fact that rapid desensitization targets mast cell degranulation via IgE saturation, while slow protocols modulate T-cell memory pathways, explains why timing and dosing intervals differ so dramatically. This is not merely empirical-it is mechanistically grounded in decades of cytokine profiling and basophil activation studies. The recent AAAI guidelines are a monumental step forward in standardizing this high-risk, high-reward intervention.
Sarah Schmidt
November 4, 2025 AT 00:20It’s funny, isn’t it? We’ve spent centuries trying to ‘cure’ allergies, yet the real breakthrough isn’t about fixing the body-it’s about tricking it. Desensitization doesn’t heal; it deceives. And maybe that’s the truth of modern medicine: we don’t fix the system, we negotiate with it. We whisper to our immune systems, ‘Just this once, pretend you don’t hate this.’ And somehow, it listens.
Billy Gambino
November 6, 2025 AT 00:00Let’s be real: desensitization is the last gasp of a broken system. We don’t have better drugs, so we make people endure hours of IV drip anxiety to use the one that works. And the fact that insurance only covers 60%? That’s not a flaw-it’s a feature. It keeps this out of reach for the working class. This isn’t progress. It’s survival theater.
Cecil Mays
November 7, 2025 AT 20:45THIS IS SO COOL 😍 I had no idea this was even a thing! My cousin just did this for penicillin and she’s now cancer-free. The whole team was like superheroes with clipboards. If this can save lives when everything else fails… why isn’t this in every hospital?! We need more of this, not less. 🙌 #MedicalMiracles
Lorena Cabal Lopez
November 8, 2025 AT 17:03They say 95% success rate. But what about the 5%? Who’s counting them? I’ve seen people get worse after this. And now they’re stuck with a drug they can’t take again… and no backup plan. This feels like gambling with your life.
STEVEN SHELLEY
November 10, 2025 AT 13:00YOU THINK THIS IS SAFE? I WORKED AT A HOSPITAL WHERE THEY MIXED THE DOSE WRONG AND A WOMAN DIED. THE NURSE WAS ON HER PHONE. THEY COVERED IT UP. THIS ISN’T MEDICINE-IT’S A TERROR RITUAL. THEY’RE USING PEOPLE AS EXPERIMENTAL SUBJECTS AND CALLING IT ‘PROTOCOL.’ YOU THINK YOUR INSURANCE COVERS THE FUNERAL? THINK AGAIN.